In most hospitals, the role of discharge planner or care transition coordinator is reserved for a nurse or other health care professional. But why? RTs with advanced credentials and degrees are a great fit for this job too, and Renato Galindo, BSRC, RRT, CPFT, is proving it.
Galindo, the lead care transition coordinator at Medical Center Hospital in Odessa, TX, explains how he landed the position.
When and why did you decide to become a respiratory therapist and where did you get your RT degree?
I was a senior in high school and was undecided as to what career path to choose. My cousin, an RT in our local hospital, invited me to shadow him for a weekend. What I saw in the ER and ICU that weekend motivated me to apply to the respiratory care program at Odessa College for my associate’s degree. I later went back for my BSRC through Midwestern State University in Wichita Falls, TX.
How long did you work as a traditional RT and what did you most like about that role?
I was a staff RT, including time as the pulmonary patient educator, for 17½ years. The various roles I was allowed to work in allowed me to grow as a communicator and as a patient advocate. I was also taught to always to think outside of the box when caring for a patient.
Why did you decide to apply for a position as a care transition coordinator and what requirements did you have to meet to be considered for the job? How long have you been working in this position?
As the pulmonary patient educator, I worked very closely with the care coordinator nurses and social workers. Their role in ensuring safe and timely discharges appealed to me. But the roles were written for registered nurses and social workers. In various conversations with the director of our community health department, we would ask why could an RT not function in that role. After careful examination, I applied and was allowed to join the team in January 2016.
What does the job entail?
Our department is a multidisciplinary department comprised of RNs, social workers, and two other RTs. As the lead care transition coordinator, I oversee a team of social workers and care transition coordinators. Our goal is to reduce length of stay and readmission rates, along with ensuring a safe discharge. Our team focuses on placement in post-acute facilities, such as LTACH, SNF, inpatient rehabs, hospice consults, etc.
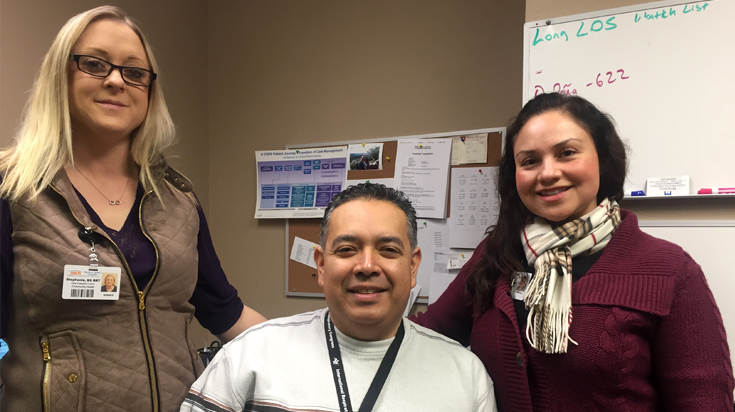
The other two RTs, Stephanie Clayton, BS, RRT-NPS, AE-C, and Martha Hernandez, BBA, RRT-CPFT, start the discharge planning process in our two intensive care units.
What do you like most about working in this position?
No two discharge plans are alike. When I was a staff RT, the focus was finishing the shift. Now I think about what the patient and their family will need a week or a month from now.
Here’s a good example. A year ago we had a 19-year-old male that was in a horse riding accident. He suffered severe head trauma and barotrauma that led to him having a PEG and trach placed. What made his case all the more difficult was that he lacked health insurance. Unfortunately, his discharge plan was to return home with family without being able to go to a post-acute facility.
The team worked with other disciplines — PT, speech, pharmacy — to cover all the patient’s needs and train his family to care for him at home. His family was able to set up outpatient rehab.
After several months of being home, he and his sister walked into the ICU to visit us. His trach and PEG had been removed and his PT had cleared him to ride horses again. After the intensivist asked him if he had not learned a lesson the first time, his response was, “Doc, you can’t be afraid of falling. If you fall, you have to get up.”
What advice do you have for other RTs who might like to pursue a similar role in their facilities?
My suggestion to other RTs is to network and get to know the discharge planners in your facilities. Do not let a job description on a job posting discourage you from applying. Sell your skills to your facility. Expand your knowledge in disease management and payment sources and work on your bachelor’s degree.
The one thing I would like everyone to consider is that this is not an easy role. We have to develop tough skin, as at times we are asked to have very difficult conversations with patients and families.
How do you think your AARC membership helped you diversify into this new role?
The AARC provides the tools we need to expand our knowledge. When I first came into the role, someone questioned if my state license allowed me to function in this role. I emailed the AARC and the liaison for government affairs promptly reviewed the job description and the state bylaws, and found that an RT license does cover this role.
Without a doubt, the AARC is a champion for all RTs.





