Lynn Butler, RRT, developed a passion for pediatric respiratory care during the ten years he spent as an RT at Children’s Medical Center of Dallas. When a local physician came to him in 2001 and asked if he had ever considered working in a pediatric practice, he was intrigued.
“He asked me to try it to see if it was a fit for me,” Butler said. “The only requirement was to be able to interact with patients and parents and have the ability to practice respiratory care independently.”
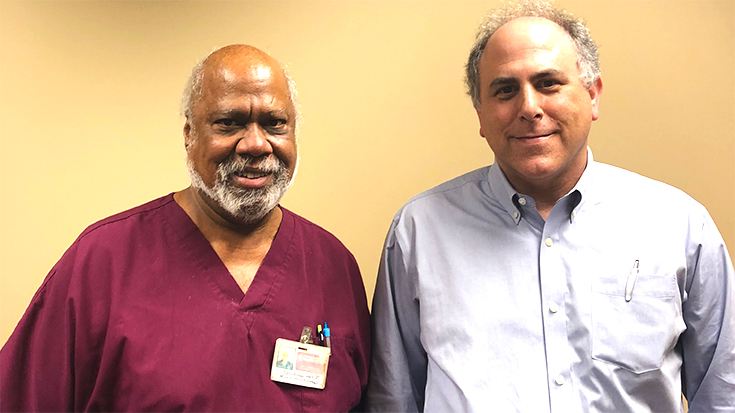
He’s been there ever since, working hand in hand with Peter Schochet, MD, and his colleagues to care for children with conditions ranging from asthma and GERD to muscular dystrophy and scoliosis.
“It can be a busy office,” he said. “There are two physicians and two respiratory therapists.”
In his blood
Butler’s main responsibilities at the pulmonology practice in Plano, TX, center around patient assessments, delivering treatments, and instructing patients and families. He and the other RT in the office also keep in contact with patients via telemedicine.
Dr. Schochet says the RTs add an important dimension to the care he is able to provide. “A nurse may be qualified for some tasks, but it would take extensive training to be as qualified as an RRT,” he said. “The respiratory therapist knows the equipment — vents, cough assist, IPV, etc. — and it is in their blood.”
The physician says he’s gotten good feedback from his patients who have received care from Butler.
“He is very knowledgeable in terms of devices, oxygen, etc. The patients like him,” Dr. Schochet said.
Challenges and rewards
According to Butler, the biggest challenge he faces in his role in the pediatric practice is keeping up with changes in respiratory medications. He also notes patience is a must in this setting, as is the ability to diffuse anxiety, fear, and apprehension in his young patients.
Those soft skills are a good indication of whether the pediatric setting is right for an RT.
“If you are destined to be a pediatric respiratory therapist, overcoming the challenges come naturally,” he said.
The biggest rewards come when he sees his patients improve as a result of his care and the teaching he does with patients and parents. “It is also great to watch the kids grow up, and when they smile at you when they come into the office and wave when they leave.”
Explore the possibilities
Butler believes there is plenty of opportunity for other therapists to work in the pediatric practice setting as well and suggests therapists who are interested in pursuing the area explore the possibilities that may exist in their communities. All it really takes is a background in pediatric respiratory care, knowledge of the disease states, and competency in the equipment being used in the office.
“If a therapist has the ability to have a friendly conversation with a physician that has a pediatric patient population, it would not hurt to ask if there could be an opportunity,” he said. Those who perform PFTs in their office or have a large population of asthma patients may have never even thought of having an RRT in house.
Dr. Schochet says physicians who decide to give it a try won’t be disappointed.
“If physicians’ offices need staff with that skill set, they would be very happy,” he said.





