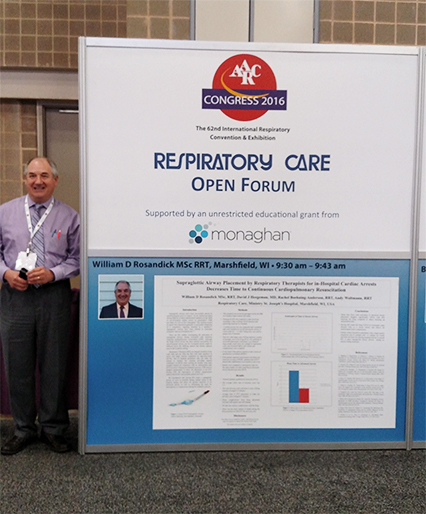
You know what they say about there being a first time for everything. For William Rosandick, RRT, an RT instructor at Mid-State Technical College and PRN RT at St. Joseph’s Hospital in Marshfield, WI, the first time to conduct a research study resulted in an abstract that was accepted into the prestigious Editors’ Choice session of the Open Forum at AARC Congress 2016 in San Antonio.
In this interview, he talks about that study and how he came to conduct it.
Why did you decide to conduct the study, “Supraglottic Airway Placement by Respiratory Therapists for In-Hospital Cardiac Arrests Decreases Time to Continuous Cardiopulmonary Resuscitation”? What piqued your interest in this topic?
RTs are not allowed to intubate at codes in our facility. Dr. David Heegeman is an ED physician who chairs the code blue review team. He is very much a proponent of continuous chest compressions. Often chest compressions are stopped to intubate. He knew that RT was at the bedside manually ventilating by BVM until the patient could be intubated. If RTs couldn’t intubate, then they should be able to place an advanced airway such as a supraglottic airway while at the bedside early at the code/cardiac arrest while not having to cease chest compressions. It was really the first research involving RTs at our hospital and it got RTs involved.
Was this your first time conducting a research study?
Yes.
What did you do to gain support from your organization to conduct the study?
In a nutshell it was communication, RT expertise, and positive results. Dr. Heegeman really was an excellent leader on this. We needed to communicate the RT’s new role to those responding to codes. This meant physicians, anesthetists, other code team members, as well as nursing care floors. We had meetings in the RT department, and he let us know he was in front of us and behind us. We had some ruffled feathers, but he made sure he addressed the need for RT to place the airways, as it was part of a study. He shared ongoing study data with the code blue team and physicians. It was easier to get support with positive results.
What were the biggest challenges you faced as you carried out the study and how did you overcome them?
The biggest challenges were making sure that all the RTs were trained to place the supraglottic airways, so we had more skill training sessions for everyone after six months of the study. Some RTs were able to place 3-4 airways and some none over the course of the study. We also needed to get and earn the support of physicians. Showing RTs could insert the airway in a timely manner with minimal complications helped win over some physicians.
How difficult was it to work the study into your normal job responsibilities and how did you alter your work routine to make it happen? Do you think it was worth the time and effort?
My main job is the DCE for our RT program at Mid-State Technical College. The study was done at St. Joseph’s, a hospital where I am a PRN RT. There was no funding, so my time was all gratis. Lots of extra time after school and on weekends. I was a little naïve, just happy to be on the team. My payment was being selected for the Editors’ Choice!
How did it feel to learn that your abstract had been accepted to the Open Forum — and most especially, that it was selected for the Editors’ Choice session?
Unbelievable! This was our first submission. We were hoping to have it selected for the Open Forum. When I received the email notification from Ray Masferrer that it was selected for the Editors’ Choice I had to reread the email a couple times to make sure I knew exactly what was happening.
How do you think conducting a study like this and having it accepted to the Open Forum is helping to further your career in respiratory care?
We have had a few institutions contact us regarding our abstract and we have shared our findings. Personally, it boosts your confidence and inspires you to do more research.
What advice do you have for other therapists who might like to follow in your footsteps but just don’t know how to get started?
Don’t wait for opportunity, create it. Originally I was not a member of the study team, but asked if they needed a hand and they said yes. I was in the process of completing my master’s degree from Northeastern University and had a few classes in research, so I figured I had some knowledge and skills to offer. Sometimes just asking a group doing a study if they need help is all it takes to get started. “No” doesn’t always mean “no” — it may be just a temporary setback.
Are you planning to conduct more studies in the future? If so, what will you study next and why?
Yes. I have been looking at 12+ years of data regarding students in our RT program and their pre-admission test scores compared to their NBRC test scores, above and below a mean score, to see if there is a correlation. Studies similar to this have been done by nursing and they found that there is some correlation, but it is not as obvious as you might think. I don’t think this has been done yet in RT and it may show the benefit of a quality RT education program and the ability to benefit students with lower pre-admission scores.





