By Dustin Money, RRT-ACCS
Several weeks ago a young respiratory therapist came to me to lament his career decision. As he sat in the chair next to mine, he said with a sigh, “I don’t know why I chose this profession!”
His frustrations were filled with all the same buzz statements I heard from others when I first entered the profession:
“Being an RT is a dead end career with no advancement.”
“Besides breathing treatments and ventilators, what else am I supposed to do with my degree?”
After giving him some time to vent, I had a simple response. “Even though I work as an ECMO specialist I am still a respiratory therapist, and if I wasn’t a therapist I wouldn’t be standing in these shoes today.”
I am proud to be an RT working in ECMO!
The patient who changed everything
When I graduated I never would have predicted that my career would take me on this amazing journey. As a new graduate I took a job as a staff therapist in the Heart Center at the University of Virginia, and over time became a senior therapist. I enjoyed being a critical care respiratory therapist.
However, one night I took care of a patient that changed my professional direction. He was a 21-year-old gentleman who developed a severe multi-lobar pneumonia and a large right sided empyema. Nothing I did with the ventilator would get this patient to oxygenate.
Right before I felt my frustration hit a boiling point a young thoracic fellow said, “Let’s put him on ECMO!”
After seven days of the right antibiotics, appropriate rest settings, and a decortication, the patient decannulated. Over the following week, the patient was liberated from the vent and was able to discharge to home.
This was the first time I saw ECMO used outside the realm of post-operative cardiac patients. I was astounded to see someone walk out the hospital who only two weeks prior was inches away from death. From that point forward I engrossed myself into learning everything I could about the technology.
Training was intense
In a nutshell, ECMO — which stands for “extracorporeal membrane oxygenation” — is a therapy utilized to support the heart and/or lungs of patients suffering from a severe disease process in which conventional therapies are not sufficient. I serve all patient populations as an ECMO specialist. This includes everyone from the newborn with meconium aspiration syndrome, to the teenaged trauma patient, to the adult patient recovering from viral myocarditis.
Some of my day-to-day job duties include building and priming blood pumps, assisting the surgeon with initiation and termination of support, formulating ventilator strategies that facilitate lung rest, transfusion of blood products, performing renal replacement therapy, and management of anticoagulation.
I joined the ECMO program at the University of Virginia as a full time ECMO specialist in 2014. Training was challenging. I underwent an intensive in-house education program, modeled after the Extracorporeal Life Support Organization guidelines for training and continuing education of ECMO specialists.
Through long didactic and practical modules, I gained advanced knowledge in a variety of areas, such as mechanical circulatory support devices, hemodynamics, circuit management, anticoagulation, pathophysiology, and mitigation of emergencies. It took several months of training and wet lab drills before I was even allowed to start sitting for clinical hours.
Challenges and rewards
Over the past three years, I have continued to advance and develop my practice in the world of extracorporeal support. I have coauthored some of my institution’s guidelines regarding adult ECMO care, become certified in the performance of ex-vivo lung perfusion (EVLP), and was part of the team that performed the first EVLP transplant in the state of Virginia.
Since becoming a specialist, I have also started utilizing my skill set with the department of surgery, working as a research assistant in the animal lab. Through my lab experience, I have coauthored several papers on porcine experiments involving EVLP, experimental lung injury, ischemic reperfusion injury, and ECMO.
As I told the young RT questioning his choice in the profession, if I wasn’t a therapist, I wouldn’t be standing in these shoes today. For those RTs looking to take the plunge into the world of ECMO, I would tell you that the career is very rewarding, though it is not without mental, physical, and emotional challenges.
Management of ECMO patients can be difficult, and it takes a skilled multidisciplinary team to care for these patients. But it is the respiratory therapist who possesses the strong foundation in cardiopulmonary critical care that helps our profession stand out in the specialist role. You must be willing to accept that the shift can be 80% routine and 20% absolute chaos. You will be called upon to help treat the sickest of the sick, and will be exposed to very emotionally charged situations. It is your job as the specialist to be the calm, cool, and collected voice in the midst of chaos.
In this career you must be a team player who is able to rely on your teammates to collectively overcome these difficult situations. To be successful in ECMO or any other career, you must be willing to be a lifelong learner and educator, as well as have the internal drive to do whatever you can to achieve growth at every opportunity you’re faced with.
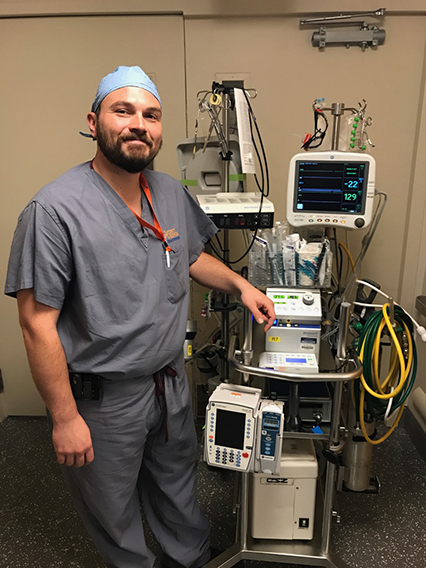
Dustin Money is an ECMO specialist at the University of Virginia Health System and a research assistant at the University of Virginia School of Medicine, both in Charlottesville, VA.





