Rising temperatures, stagnant high-pressure domes, and trapped air pollutants are becoming more common in the United States. This was particularly evident this summer in the West and Northwest U.S. making it clear we need to be aware of the threat that heat and poor air quality pose for our patients with chronic pulmonary disease. Unfortunately, the extraordinary has become ordinary as the average ambient temperature has continued to rise since 1980, reaching its highest level in 2016 and 2020 (See Figure 1). This trend will likely continue despite our best efforts to mitigate the ambient temperature rise. Therefore, a deeper understanding of the risks is needed to best educate our patients and prepare them to deal with this evolving challenge successfully. In this review, I plan to discuss the basics risks of excess heat, the impact of heat and poor air quality on respiratory health, the added challenges posed by wildfire smoke, and some measures to advise those with chronic respiratory disease.
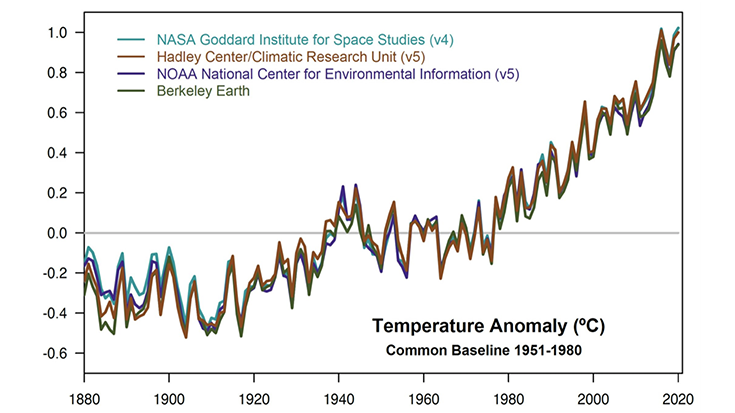
Figure 1. Average ambient temperatures from several reliable sources since 1880. Data from the National Aeronautics and Space Administration (NASA)
Types of Direct Heat Related Illnesses
Heat related illness can result from direct injury by failure to regulate body temperature due to failure of normal thermoregulatory mechanisms, particularly as the ambient temperature rises above normal body temperature and humidity limits the ability to dissipate heat via evaporation.1 This type of direct heat injury in its most dangerous form results in heat stroke, in which dangerous hyperthermia (core temperature > 105oF is combined with central nervous system signs such as altered mental status, confusion, seizures, and coma. Heatstroke is often accompanied by tachycardia and hypotension from the depletion of intravascular volume and vasodilation. Heatstroke is a critical care emergency and requires immediate measures to cool and admission to a hospital.2 Heatstroke activates an intense inflammatory response like septic shock and can result in multi-organ system failure and ARDS3 if not promptly treated with active cooling. Heat exhaustion is a less severe form of direct heat injury but needs prompt attention as it can progress to heatstroke. Heat exhaustion is characterized by high temperature, cold clammy skin, thirst, headache, and fatigue, but victims are clear-headed with only some lightheadedness and headache. Treatment for the victim includes moving them to a cool shady spot, elevating the legs, rehydrating, and cooling with cool, wet surface contact and evaporation. Patients should be taken to the Emergency Room for electrolytes and possible intravenous rehydration, but they can usually be discharged after several hours.2 Less severe forms of direct heat stress include sunburn, heat rash, and muscle cramps. People at risk for direct heat injury include those at the extremes of age, who have less active thermoregulatory systems, those who have taken alcohol or other drugs that impair temperature regulation, people who work outdoors, and athletes. Prevention and awareness of the risk are keys to avoiding this set of heat injuries. The CDC has a useful patient education tool that visually addresses how to stay safe in extreme heat events.
The U.S. Global Change Research Program describes how we initially found an association between extreme heat events and respiratory disease with observations of severe heat waves in Kansas City and St. Louis (1980), Chicago (1995), and California (2006). We learned more about this relationship with more extensive cohort studies in Europe4,5 and the United States6, which showed that admissions for respiratory symptoms and deaths were correlated with heat events. The population most affected were the elderly with chronic respiratory and cardiovascular disease, but no direct mechanism was identified. For respiratory disease mechanisms Michelozzi et al.4 postulated that patients with chronic respiratory disease might have impaired thermoregulatory systems. They may hyperventilate and create more dynamic hyperinflation, or there may be activation of pulmonary vasoconstriction. Increased mortality was seen more in urban environments, but there was considerable geographical variation. Heatwave intensity and duration have an impact, but the correlation with intensity is somewhat stronger.7
Air Quality & Indirect Heat Related Illness
Air quality contributes greatly to the acute and chronic burden of disease, and air quality deteriorates significantly in extreme heat events. Natural and human sources generate a wide variety of air pollutant chemicals; the CDC monitors6 for air quality including: carbon monoxide, lead, nitrogen oxides, ozone, particulate matter (PM), and sulfur dioxide. The pollutants contributing to the Air Quality Index (AQI) are ozone and fine particulate matter. The fine particulate matter is defined by particle size, with PM2.5 being particles less than 2.5 microns and PM10 less than 10 microns. Particulate matter comes from various sources, but the combustion of carbon-based materials produces the majority. PM2.5 is used in the AQI and quantified as micrograms per cubic meter of air inhaled with <12.5 ug/m3 considered safe, and ozone is quantified by parts per million, with 0.070 ppm considered safe according to the 2015 EPA guidelines. Note that a patient with higher minute ventilation (MV) exposes themselves to a greater amount of PM. Hence, the added burden of exposure to those who exercise and those with elevated dead space like our COPD patients. A New England Journal of Medicine (NEJM) landmark study in 20178 used the Medicare database with over 60 million patients followed for 13 years and correlated mortality and local ozone and PM2.5 levels from across the continental United States. The NEJM study authors found a direct strong positive correlation between levels of ozone and PM2.5 with overall mortality even at levels considered safe by the AQI. This effect was more pronounced in Black men and in high Medicaid use (lower socioeconomic status). They found that ozone was the dominant pollutant in the Western U.S. and PM2.5 more active in the Eastern U.S. A subsequent study using the same model demonstrated a similar positive correlation of mortality with PM10.9
Severe heatwaves are usually associated with high-pressure systems that stagnate over geographical regions, as we saw in the Northwest in 2021 A meteorologic system known as a “heat dome”10 develops. It traps air pollutants such as ozone, fine particulate matter (PM2.5), carbon monoxide, nitrogen dioxide, and sulfur dioxide generated on the earth below the heat dome. As the gasses in the high-pressure system heat up, they expand vertically into the troposphere, and low-pressure systems and cool fronts cannot displace the heat dome. The stagnant hot air traps the air pollutants, and air quality deteriorates. Ozone and fine particulate matter accumulate to very high levels, and they are bad actors in the airways. Ozone is a reactive oxygen gas composed of three oxygen molecules. Ozone high in the earth’s stratosphere is beneficial as it serves as the sunblock for the earth, blocking UV rays that can be harmful. Ozone at lower levels of the atmosphere (the troposphere) is produced by the reaction of nitrogen oxides with reactive organic compounds in the presence of heat and sunlight. (See Figure 2) When ozone and PM2.5 are inhaled, they initiate inflammation in the airway, bronchoconstriction, and mucous production, and patients complain of chest tightness and cough within a few hours of exposure. Short term exposures to ozone and PM2.5 have been shown to increase asthma-related emergency room visits and hospitalizations.11
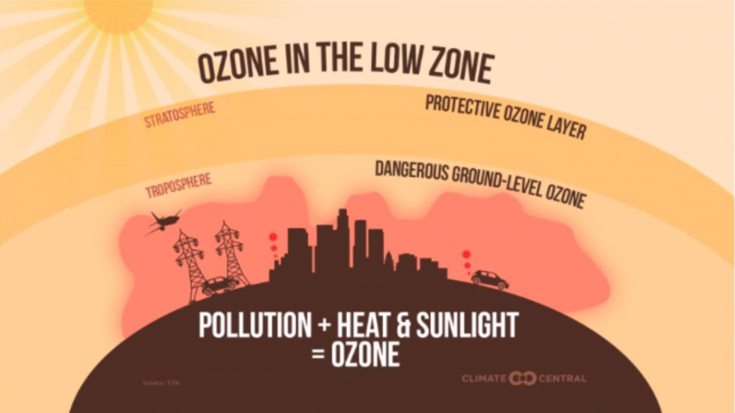
Figure 2. Graphic demonstrating how heat domes trap ozone in the lower levels of the atmosphere.
Most of the research done on heat and air quality related to health outcomes deals with overall mortality, which combines the multi-organ system effects of both heat and pollution. Respiratory mortality is a large part of that burden. Still, we must look to more specific studies to get a window on the impact of these events on patients with pulmonary disease. Much research has come from China, which went through a tremendous change in air quality as it has industrialized over the past 30 years and produced some of the worst conditions for air quality in the early 21st century.12 They have initiated many measures to combat air pollution but still have more to do. In a systematic review of the China experience, Guan et al.12 described the cost of poor air quality in years of life lost and the economic burden. They make a strong case for active measures to reduce the human and economic burden. The research in China demonstrated a strong correlation between the incidence of chronic respiratory disease and lung cancer measures compared to metrics for air quality in a dose dependent manner. They describe significant improvements since more stringent measures were taken in the early 2000s.
Outdoor air quality and temperature are important considerations, but many of our patients with chronic respiratory conditions spend most of their time indoors. McCormack et al.13 performed a longitudinal cohort study involving 69 patients with moderate to severe COPD and correlated indoor temperature and levels of common air pollutants with symptoms, inhaler use, and spirometry over 601 patient days during the warm season in Baltimore. They found that increased indoor temperature was associated with worsening scores for breathlessness, cough, and sputum production. Elevated levels of NO2 and PM2.5 magnified the effect. There was a significant increase in inhaler use with elevated temperature and elevated PM2.5 and NO2, but evening and morning spirometry were unchanged. The important take away is that indoor air temperature and air quality are important considerations in advising our patients. Heather Wilden interviewed Mike Hess, MPH, RRT, RPFT for the AARC Newsroom in 2019 and described how our energy efficient homes trap and concentrate ozone, nitrogen dioxide, particulate matter, smoke and dander.
Impact of Wildfire Smoke
We’ve seen a tremendous increase in wildfires in the past decade across the globe. Wildfire season in the U.S. is longer, with more severe fires and more acreage consumed. These fires are more difficult to control as they get larger and generate their own local fire-related phenomena that make the fires more explosive. Wildfires generate the same chemical pollutants we have discussed above but in much larger concentrations throughout the exposure. Wildfires produce much more particulate matter depending on proximity to the fire and may have added petrochemicals depending on structures, vehicles, or businesses consumed in the fire.
The research on the health impact of wildfires focuses on observational studies of health outcomes in affected areas. The data supporting a link to asthma exacerbations is the strongest. Several studies have shown bronchospasm in patients without a history of asthma, and rescue inhaler use, related emergency room visits, and hospital admissions for asthma have been shown to increase in areas affected.14 The evidence regarding COPD exacerbations is more mixed. Initial observational studies of the local impact of wildfires on COPD outcomes showed a strong association between exposure to wildfire smoke and acute exacerbations of COPD, but recent studies have not been as clear in establishing a relationship.15 It may be that we are getting better at mitigating the effects through better communication and public health measures. There have been reports of increases in lower respiratory tract infections which appear somewhat later after the exposure, but this requires more study.
Education of Patients and Public
One of the keys to helping our patients is increasing awareness, which will help them take appropriate preventative measures and maintain health during summer heat spells and local air quality alerts. Following local weather forecasts can be enough to be aware of local weather. Still, I have found that weather monitoring apps can be beneficial with timely alerts to guide activity. For example, one of favorites provides heat advisories, alerts to lightning and other dangerous phenomena, and the weather radar. For air quality, most weather apps will give air quality warnings. Still, I find the EPA site AirNow.gov is a quick, easy source that localizes the report to your zip code and has excellent information about air quality.
Advice to Prevent Heat Related Illness: The CDC provides an excellent pamphlet for patient education for the prevention of heat related illness. They advocate a variety of common-sense measures. These measures include minimizing time outdoors, using air conditioning or spending time in air-conditioned spaces, minimizing use of heat-generating indoor devices like the stove, staying hydrated with water or beverages that don’t contain caffeine, sugar, or alcohol, using a fan when the ambient temperature is less than 95oF, and eating light cool easy to digest meals. They also advise us to watch out for high-risk groups like the elderly, disabled, and those with chronic disease. Outdoor workers should be aware of early signs of heat exhaustion, work with partners, take frequent hydration breaks, and wear light-colored, loose-fitting clothing. Athletes should exercise early in the day, watch out for each other, and find ways to bring workouts indoors.
Advice to Deal with Poor Air Quality Days: The American Lung Association (ALA) provides excellent information for the public on air quality and is a great way for clinicians to get involved in advocacy for improving air quality through its Health Air Campaign. The ALA provides a list of 10 tips to protect oneself from poor air quality. These tips include staying on top of the air quality using tools like AirNow.gov, minimizing time outdoors, avoiding exercise in high traffic areas, using less energy in your home, and not contributing to the problem with the use of gas-powered lawn equipment or outdoor burning, and minimizing time driving. In addition, the ALA tips encourage parents to get involved with measures to minimize student exposures to school bus emissions, which are a big source of PM10.
Advice on Managing Indoor Air Quality: The American Thoracic Society has a great patient education pamphlet for managing indoor air quality. The ATS guidance addresses general measures to ensure minimal exposure to irritants, triggers, and pollution. Carlsten et al.16 recently provide a great summary of the evidence to inform providers and the public on improving air quality. The authors review the evidence supporting using a well-fitting N95 mask when outdoors and using indoor air processors with HEPA filters, electrostatic filters, or activated carbon to reduce indoor air pollutants. The Carlsten et al. systematic review also nicely summarizes the early evidence that shows protection from a diet rich in antioxidants and vitamins C and E.
Advice on Dealing with Wildfire Smoke: The ATS provides a patient education pamphlet advising patients with chronic pulmonary disease on managing their health during a wildfire event. For those in wildfire areas, they recommend planning early evacuation if possible, establishing a clean room with recirculating air conditioning or an air purifier, and making sure they follow their care plan and have backup meds as needed. When in a situation where wildfire smoke is thick, and AQI is low, they recommend staying indoors and wearing a well-fitting N95 mask when they have to go out. The ATS advises minimizing other indoor air pollution, limiting cooking, and avoid vacuuming. When a person with a respiratory disease has to travel in a vehicle, it should be with windows closed and air conditioning on with recirculation if possible. They advise using air purifiers with HEPA filters and avoiding ionic or oxygenators that can produce ozone.
Advocacy
The final point I would like to address is the importance of advocacy from respiratory clinicians in our pursuit of clean air policies that will improve the lives of our patients. The voices of health care personnel can make a difference as we can bring the real-life health impact of heat, poor air quality, and wildfires to the attention of the media and government officials. Respiratory therapists should be experts in this area, and I strongly advise you to volunteer to discuss the topic with the media and other venues. It helps inform the public, and it raises the profile of respiratory therapy in the community. An excellent example of this type of advocacy was an ATS Workshop Report from 201217, which described an effort by the ATS to bring together experts from vital professional societies and government agencies to identify areas that must be addressed if we are to make an impact. They came up with 27 recommendations we can take now to adapt and mitigate, and critical areas that need more research. As we saw in the United States after the Clean Air Act of 1970, we can improve air quality and reduce the attendant disease burden. A wonderful recent report from the Environmental Committee of the Forum of International Respiratory Societies (FIRS)18 details how local, regional, national, and worldwide efforts have impacted health outcomes. We can change the dangerous arc of this problem, and it will save lives, decrease morbidity and be economically advantageous. We all need to jump off the sidelines and into the fray.
References
- Cheshire WP Jr. Thermoregulatory disorders and illness related to heat and cold stress. Auton Neurosci 2016;196:91-104. doi:10.1016/j.autneu.2016.01.001
- Gauer R, Meyers BK. Heat-Related Illnesses. Am Fam Physician 2019;99(8):482-489. Retrieved from: https://pubmed.ncbi.nlm.nih.gov/30990296/
- el-Kassimi FA, Al-Mashhadani S, Abdullah AK, Akhtar J. Adult respiratory distress syndrome and disseminated intravascular coagulation complicating heat stroke. Chest 1986;90(4):571-574. doi:10.1378/chest.90.4.571
- Michelozzi P, Accetta G, De Sario M, D’Ippoliti D, Marino C, Baccini M, et al. High temperature and hospitalizations for cardiovascular and respiratory causes in 12 European cities. Am J Respir Crit Care Med 2009;179(5):383-389. doi:10.1164/rccm.200802-217OC
- Iñiguez C, Royé D, Tobías A. Contrasting patterns of temperature related mortality and hospitalization by cardiovascular and respiratory diseases in 52 Spanish cities. Environ Res 2021;192:110191. doi:10.1016/j.envres.2020.110191
- Medina-Ramón M, Schwartz J. Temperature, temperature extremes, and mortality: a study of acclimatisation and effect modification in 50 US cities. Occup Environ Med 2007;64(12):827-833. doi:10.1136/oem.2007.033175
- Xu Z, FitzGerald G, Guo Y, Jalaludin B, Tong S. Impact of heatwave on mortality under different heatwave definitions: A systematic review and meta-analysis. Environ Int 2016;89-90:193-203. doi:10.1016/j.envint.2016.02.007
- Di Q, Wang Y, Zanobetti A, Wang y, Zanobetti A, Koutrakis p, et al. Air Pollution and Mortality in the Medicare Population. N Engl J Med 2017;376(26):2513-2522. doi:10.1056/NEJMoa1702747
- Liu C, Chen R, Sera F, Vicedo-Cabrera AM, Guo Y, Tong S, et al. Ambient Particulate Air Pollution and Daily Mortality in 652 Cities. N Engl J Med 2019;381(8):705-715. doi:10.1056/NEJMoa1817364
- Climate Central. Climate change is threatening air quality across the country. https://ccimgs-2019.s3.amazonaws.com/2019AirQuality2/2019AirQuality.pdf. July 31, 2019. Accessed July 23, 2021.
- Zheng XY, Ding H, Jiang LN, et al. Association between air pollutants and asthma Emergency Room visits and hospital admissions in time series studies: A Systematic Review and Meta-Analysis. PLoS One 2015;10(9):e0138146. Published 2015 Sep 18. doi:10.1371/journal.pone.0138146
- Guan WJ, Zheng XY, Chung KF, Zhong NS. Impact of air pollution on the burden of chronic respiratory diseases in China: time for urgent action. Lancet 2016;388(10054):1939-1951. doi:10.1016/S0140-6736(16)31597-5
- McCormack MC, Belli AJ, Waugh D, Matsui EC, Peng RD, Williams DL, et al. Respiratory Effects of Indoor Heat and the Interaction with Air Pollution in Chronic Obstructive Pulmonary Disease. Ann Am Thorac Soc 2016;13(12):2125-2131. doi:10.1513/AnnalsATS.201605-329OC
- Reid CE, Brauer M, Johnston FH, Jerrett M, Balmes JR, Elliott CT. Critical Review of Health Impacts of Wildfire Smoke Exposure. Environ Health Perspect 2016;124(9):1334-1343. doi:10.1289/ehp.1409277
- Reid CE, Maestas MM. Wildfire smoke exposure under climate change: impact on respiratory health of affected communities. Curr Opin Pulm Med. 2019;25(2):179-187. doi:10.1097/MCP.0000000000000552
- Carlsten C, Salvi S, Wong GWK, Chung KF. Personal strategies to minimise effects of air pollution on respiratory health: advice for providers, patients and the public. Eur Respir J 2020;55(6):1902056. Published 2020 Jun 4. doi:10.1183/13993003.02056-2019
- Pinkerton KE, Rom WN, Akpinar-Elci M, Balmes JR, Bayram H, Brandi O et al. An official American Thoracic Society workshop report: Climate change and human health. Proc Am Thorac Soc 2012;9(1):3-8. doi:10.1513/pats.201201-015ST
- Schraufnagel DE, Balmes JR, De Matteis S, Hoffman B, Kim WJ, Perex-Padilla, et al. Health Benefits of Air Pollution Reduction. Ann Am Thorac Soc 2019;16(12):1478-1487. doi:10.1513/AnnalsATS.201907-538CME
Email newsroom@aarc.org with questions or comments, we’d love to hear from you.