Since its inception, the AARC has been supported by physicians invested in ensuring the success of the profession. Today, our Board of Medical Advisors (BOMA) includes representatives from major medical societies and other organizations with an abiding interest in respiratory care. It is led by a chair who oversees the board and works closely with leaders in the AARC to advocate for mutually beneficial outcomes.
 Promoting greater use of RTs outside the hospital will be a crucial goal for Dr. David Bowton during his term as chair.
Promoting greater use of RTs outside the hospital will be a crucial goal for Dr. David Bowton during his term as chair.2022 brings a new chair to the helm in the person of David L. Bowton, MD, FCCP, FCCM. A seasoned member of BOMA, Dr. Bowton is Professor Emeritus in the Section on Critical Care in the Department of Anesthesiology at Wake Forest School of Medicine in Wake Forest, NC. During his tenure at Wake Forest Baptist Health, he served as medical director of respiratory care. He has authored numerous papers in peer-reviewed journals related to the provision of care to people with respiratory conditions.
In this interview, Dr. Bowton talks about his long involvement with the respiratory care profession and his vision for BOMA going forward.
When and why did you first become interested in pulmonary medicine?
I became interested in pulmonary toward the end of my residency in internal medicine, though at the time-critical care was not a recognized specialty. I was influenced by the example of my chief resident, Ed Haponik, and by faculty mentors who applied physiologic principles to the management of the very sick.
What do you believe have been your most important contributions to pulmonary medicine over your long career, and why do those stand out in your mind?
Mentoring, teaching, learning from, and working with pulmonary and critical care fellows, residents, respiratory care practitioners, nurse practitioners, and physician assistants have been the most personally rewarding aspects of my career. Our publications establishing the benefits of protocolized liberation from ventilator support directed by respiratory care practitioners stand out as key contributions — Ely EW, et al. N Engl J Med. 1996; 335(25):1864; Ely EW, et al. Am J Respir Crit Care Med. 1999;159(2):439).
You served as medical director of respiratory care at Wake Forest Baptist Health from 2003 to 2013. What did you learn from that experience about the value that RTs add to the health care team, and how have you advocated for respiratory therapists both at Wake Forest and in the larger health care community?
During my long working relationships with RTs, I have seen their commitment to high-quality patient care and service as invaluable resources to their colleagues. Their efforts improve patient outcomes, provide valuable patient education, and offer insight into optimal patient management for their colleagues.
At Wake Forest, we were an early adopter of respiratory therapist-driven protocolized care, which reduced unnecessary or ineffective therapies and increased the delivery of appropriate care to patients. The success of this program increased the visibility of our respiratory therapists and highlighted their value to improved patient outcomes and cost-effective care.
When did you first become a member of the AARC’s Board of Medical Advisors, and what led you to accept the appointment on behalf of the American College of Chest Physicians?
I became a member of BOMA in 2015. I have actively supported physician engagement with the profession of respiratory care, serving as president of the Commission on Accreditation for Respiratory Care, chair of the Respiratory Care Network Steering Committee of CHEST, and as a member of the Advisory Board of the UNC Charlotte Respiratory Care Program.
I was eager to accept the opportunity to directly engage with leaders of the AARC by serving on BOMA.
How do you believe physicians can partner with the AARC through BOMA, and how can they advocate for RTs?
The members of BOMA, through their supporting organizations, can leverage the AARC’s impact on legislators at the state and national level and with insurers to advance the practice and reimbursement of respiratory care practitioners. BOMA can also provide the AARC with additional insight into physicians’ perceptions of how RTs directly impact physicians’ practice and patient care.
How can physicians help lead the charge for RTs to work outside of the hospital setting, and why is this important for patient care?
Physicians can insist that RTs supervise the patient education and set up of all home respiratory care services and, whenever possible, utilize only DME providers that utilize RTs in this manner. Pulmonary rehabilitation services are not widely available and are under-prescribed, yet have been repeatedly shown to be both cost-effective and improve the quality of life of patients with pulmonary diseases. The AARC and BOMA can help to educate the public and health care providers about the value that RTs provide in outpatient education, outpatient evaluation and treatment, and organization and delivery of pulmonary rehabilitation services.
What do you believe are the most valuable services RTs provided to your own patients over your long career, and why?
The RT-physician relationship is a symbiotic one. RTs have a unique knowledge base that amplifies physicians’ ability to effectively care for their patients with respiratory diseases.
RTs have played a vital role in educating my patients — helping them understand the appropriate use of their medications and how to administer them correctly. Over the last 20 years, my practice was focused on critical care, and RTs were indispensable in being the first to recognize changes in patients’ conditions, coordinate the liberation from mechanical ventilatory support, and ensuring the appropriateness of respiratory care therapeutics.
What will be your primary objectives for BOMA during your term as chair, and why are these objectives most important to you and the board at this time?
My major objectives are to increase substantive interactions of BOMA with AARC leadership and to more effectively engage our supporting organizations and their members to communicate the message that the knowledge and skills of RTs are essential to the provision of high-quality patient care.
Over the longer term, my hope is that these efforts will result in educational and practice opportunities that broaden RT expertise and scope of practice and increase RT compensation.
Following your recent retirement, you were named Professor Emeritus in the Section on Critical Care in the Department of Anesthesiology at Wake Forest School of Medicine. How will you be staying active with the university and your research interests in retirement, and why is it important to you to do so?
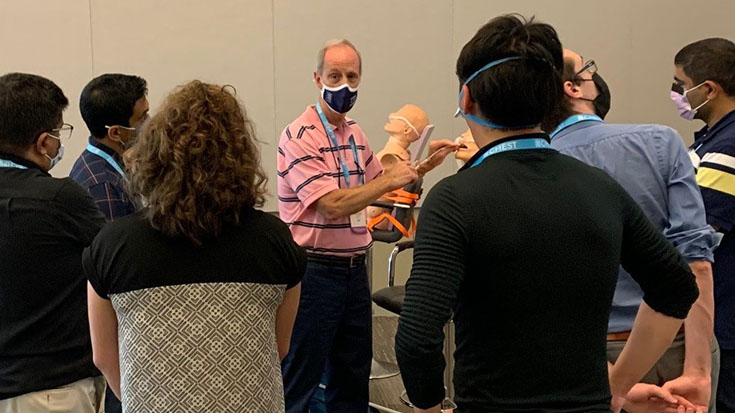
I still provide, and hope to continue to provide, didactic and simulation education for our critical care trainees in the areas of airway management and mechanical ventilatory support. I remain active in CHEST educational efforts both at the annual meeting and in CHEST-sponsored simulation courses. There hasn’t been a course or teaching session when I haven’t learned something. These interactions give me immense satisfaction and provide structure and purpose to my retirement.
Email newsroom@aarc.org with questions or comments, we’d love to hear from you.














