The Newly Charted Horizons
Several years ago, the health care organization I worked for underwent the transition to a new Electronic Medical Record (EMR) system. The organization consisted of over 20 hospitals across two states in Utah and Idaho. The implementation of this system was supported by increasing the number of staff, additional training, and on-site technical support. As each hospital in the system transitioned to the new EMR, each “go-live event” had fewer issues. However, the challenge of changing to a new EMR system was equivalent to hiking Mount Everest. The experience served as a gateway to a whole new set of challenges for many clinical departments.
Growing pains of change
Less than four months after the initial transition, operational challenges started to arise.
Implementing a new EMR had turned tenured experts into beginners. While the processes of clinical care had not changed, the documentation system was completely different. This new environment caused confusion, slowdowns, missed charges, and overall inconsistent documentation. This experience may be similar to any organization that changes a cornerstone of clinical operation, with the impact of such change lasting years later.
Reconciling challenges lead to a new journey
One of the more significant challenges came from reconciling budgets and productivity. Within four months of the “go-live event” at the hospital I worked at, the respiratory care department was off its financial targets by over 30%. The financial impact started to slow down and impeded other improvement goals as cost-cutting measures started to occur. The local department leadership met to investigate the issues and try to create a solution that would better align the new EMR system with productivity targets.
Another three months passed with a variety of tactics and tracking systems implemented with no effect.
Trying to fix the problem meant more manual tracking and collaborating with our financial planning teams. It would require a systematic and team-based approach. That is where the journey of productivity tracking using a time-value tracking system started.
A New Type of Compass
The flood of new information technology into the health care field changes clinical operations. The old methods of tracking on paper and self-reporting lacked any advantages over the new data-driven strategies. Getting a hold of the massive amount of data collected by new EMR systems was the first step to solving our hospital’s problems.
Luckily, the EMR system could access and report data fields directly from the EMR. Once we developed the data queries and designed reports, the next step was to learn from the data and how it could assist in a new time-value-based system.
Raw data and information are not the same things. Raw data is like an assortment of ingredients for a meal. Without proper assembly, the outcome will taste horrible. Similarly, raw data that is appropriately prepared can become information that leads to operational success.
Our department was able to pull a report with every respiratory therapist’s daily charges, with details like time, unit, room number, and activity. This data alone did not explain how or why we met the budget. The data required processing using a time-value-based system to assess product performance. We had to pull raw data and apply specific metrics, requiring several steps to transform raw data into a time-value-based system. These elements were first connected using basic excel programing and an introductory understanding of data analytics.
Starting with raw data, rather than finance-generated reports, managers could design a more granular set of information. We structured the raw data reported from the EMR as follows:
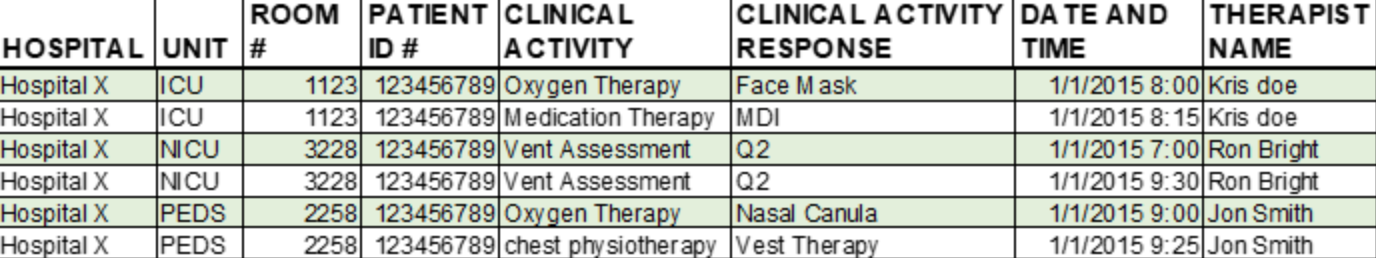
(Picture is fabricated to avoid PHI concerns)
With each line of data showing a single clinical activity, managers could visually review the work completed during a shift. If we were to count each line as requiring the same amount of clinical work, then the totals per therapist would not reflect the amount of clinical work or time-value of the RT for each shift.
However, this is where the first hurdle arises. Not all clinical activities are the same in terms of the time-value they provide, or the duration of time required to administer care. A single MDI administration does not take the same amount of time as a ventilator assessment. Giving weight to each activity based on the time allowance is not a new idea. The use of these weighted systems is also used in managing physician time-value in the health care environment. They are commonly called Relative Value Unit (RVU) weighting systems and are the backbone of productivity tracking systems. Attaching these weights to each row of data allowed for every RT’s workload to be measured based on the actual time-value instead of a total number of charges generated. The new data format would include these RVUs.

(Picture is fabricated to avoid PHI concerns)
By including weighted data to determine individual time-value generated by each RT, the department had a way to see workload-value in real-time. Like a compass pointing north, this data helps provide a clear direction to set operational goals. Measurement of each RT’s Value per shift allowed leadership to establish an operational goal of 1,000 RVUs per RT per shift. This target was created to account for all operating expenses, including non-clinical overhead.
To help keep staff on task, shift supervisors would track the workload data throughout the day and manage to staff accordingly. More importantly, this type of data tracking allowed for greater exploration into department operations.
Making The Map
An extensive collection of raw data and weighting it for workload value will not automatically explain why budget or operations are missing targets. Once the system is operational, our leadership team had more questions than answers. A leadership meeting was held to collect feedback from front-end staff. Several key questions needed answers to help improve operations.
- Do we agree that the RVU values are fair?
- Is the 1,000 RVU goal achievable with all workloads?
- What units and people are the most productive?
- What tasks are performed most and least?
- What should be done when workloads don’t meet the productivity goals?
The RVU time-values being used were validated by our hospital organization and matched with the American Association of Respiratory Care’s (AARC) Uniform Reporting Manual (URM) published standards. Assuring staff of those standards helped prevent push-back on the numbers being reported. Once people started to trust the numbers, they understood and agreed with the goals. Many staff members wanted to know their productivity and competed for higher values. Using more department-created tools tracking unit productivity allowed us to dive into each hospital floor’s specific workload differences. Just as ICU and Med/Surg floors have a different understanding of patients, they also have variations in treatment orders and care frequencies.
It was not until a full year after the EMR implementation, and we first started down the productivity journey, that systems were fine-tuned and applied with some acceptance. We had mapped out all the different variations of staffing, productivity, and workload divisions. A new baseline had been created with evidence to support each change made to workloads and staffing. As nothing in the clinical environment is fixed, the system’s daily tracking and continued management must be maintained. The continued use of this program has paid dividends time after time.
Lessons Learned
In the years after our EMR implementation and initial budget challenges, the respiratory care department has used these tools to overcome other operational challenges—this time-value system allowed for cross-comparison with benchmarking metrics and allowed for a more granular look at improvement. Telling clinical staff to work harder or chart more may have a short-term bump in productivity but does not generate reliable improvement. The most significant value added to department operations was the culture change. The staff started to acknowledge productivity goals and tried to innovate daily activities to help achieve them. This collaboration creates a more consistent approach to productivity management.
Maintaining confidence in the productivity tracking and value-based approach requires the opportunity for staff inquiry. In our department, staff members are encouraged to ask questions about productivity measurement, goals, and the tactics used in daily operations. There is always room for improvement when it comes to these foundational tools. Continued investment into our established programs will continue to support growth in our clinical operations.
Email newsroom@aarc.org with questions or comments, we’d love to hear from you.