
The Life Care Center of Kirkland in Kirkland, WA, was the face of the COVID-19 pandemic for the U.S. in the early days of the outbreak. According to news reports, at least 35 residents in the facility died from the virus, and two-thirds of the residents and dozens of staff members were infected.
Evergreen Health Medical Center in Kirkland was one of the first hospitals to receive cases from the facility. Susan Wright, BA, RRT, AE-C, is a staff therapist at the hospital working mainly in the CCU and has been on hand since the ordeal began.
Progressive care
“We received our first patients on about Feb. 28 from Life Care Nursing Home and most of the patients were admitted to our hospital,” Wright told us on Friday, Apr. 3. “To date, we have had approximately 50 ventilated COVID patients, with six weaned. None of the six have been discharged from the hospital as of this week.”
The age range of patients being treated at the hospital has changed since the earliest days of the pandemic.
“After the initial wave of elderly patients from the nursing home in Kirkland, we are seeing younger patients with few or no pre-existing conditions,” she said. “Diabetes is a predominant condition.”
Patients are presenting with high fevers, 38-40 C, high CPK, and their CXRs show bilateral patchy infiltrates.
According to Wright, they are receiving progressive care from pulmonologists who follow the ARDSnet protocols.
Ventilation is started with heated wire circuits, and Aerogen nebs are given. They are using VC and high PEEP maintained with PEEP ladder. When high FIO2 and PEEP have been maximized, 6cc/kg Vt. prone ventilation is implemented.
Sedation is achieved with fentanyl, propofol, and presidex. The unit turns to paralytics only if needed, and then for as short a duration as possible.
“Due the severely weakened condition of the surviving patients, the doctors are trying to reduce sedation as much as possible,” Wright said.
Secretion clearance
Secretion clearance is key in caring for these patients. Wright says secretions are thick, sticky, and gelatinous, and they are generally creamy as well, ranging in color from a pink tinge to dark old bloody plugs.
“We have tried hypertonic saline nebs with little success,” Wright said. “I am finding saline lavage works best to mobilize them.”
She has also found that when dark secretions appear on the tip of the inline suction catheter, a plug is generally found near the tip of the ETT.
“Breath sounds do not always reflect a plug,” she emphasized.
Wright and her colleagues have found that CPT is not effective with these patients, nor is BIPAP. They are using high flow nasal cannulas both pre- and post-extubation.
When the measures they can take in their CCU are not enough, they are turning to more sophisticated forms of life support.
“We have sent three of the patients out for ECMO, one weaned and extubated,” Wright said. “They were under the age of 55.”
For patients who go into renal failure, dialysis is considered.
One to two weeks
For most of the patients they have seen, one to two weeks of ventilation is typical, and Wright says physicians are up front with families about the low probability of survival if ventilation is initiated.
However, once extubated, the recovery process begins. Wright says all the patients have been incredibly weak post extubation and staff are using CCU mobility as much as the patient can tolerate.
Some patients at Evergreen Health are also receiving treatment with one of the promising drugs for COVID-19.
“Our facility is part of a double-blind clinical study for Remdesivir,” Wright said. “Most of the patients that have weaned off the ventilator are in the trial.”
Extra precautions
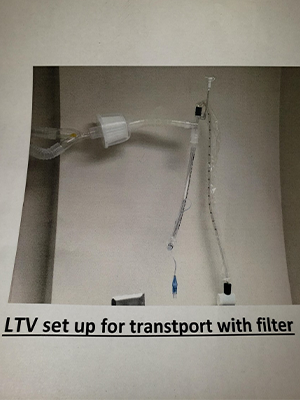
Keeping staff as safe as possible during this crisis is paramount for the hospital and Wright says they have taken some extra precautions that may be of interest to her fellow RTs. Those are illustrated in the two photos appearing with this article.
The first photo shows the addition of a Hepa filter on the resuscitation bag and transport vent circuit to protect the staff.
“The second picture shows the sign we place on room doors when an aerosol generating event occurs,” Wright said. “The stop sign is turned out and an end time is written on it to notify staff when it is safe to enter the room with a standard mask.”
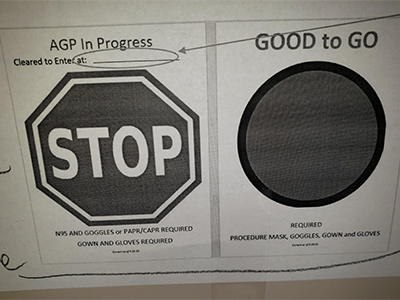
The stop sign remains in place for 23 minutes after the procedure is completed. Only then is the sign turned to the green ”good to go” side to let staff know it is safe to enter the room.
Get ready for a long haul
News reports over the past week have indicated Washington State may be flattening its curve, and Wright says evidence of that has been seen at her hospital.
“Over the last week we have noticed a slight plateau of new ventilators,” she said.
She notes her state has been on a stay-at-home order for almost a month, along with social distancing, and while she can’t be sure, her hope is that these measures are making a difference. As for her colleagues in other states that have yet to see a peak in cases, she advises them to stay safe and take care of each other. But she emphasizes it will be a marathon, not a sprint.
“Be prepared for a long haul,” Wright said. “I have been a therapist since 1982 and this is the most deadly virus I have encountered.”
Email newsroom@aarc.org with questions or comments, we’d love to hear from you.












