
When the COVID-19 vaccines started to roll out late last year, hopes were high that the pandemic would soon be a reflection in our rearview mirror. But more than six months later, it’s still here. In areas of the U.S. with low vaccination rates and extensive spread of the significantly more contagious Delta variant, respiratory therapists feel like they are back to square one.
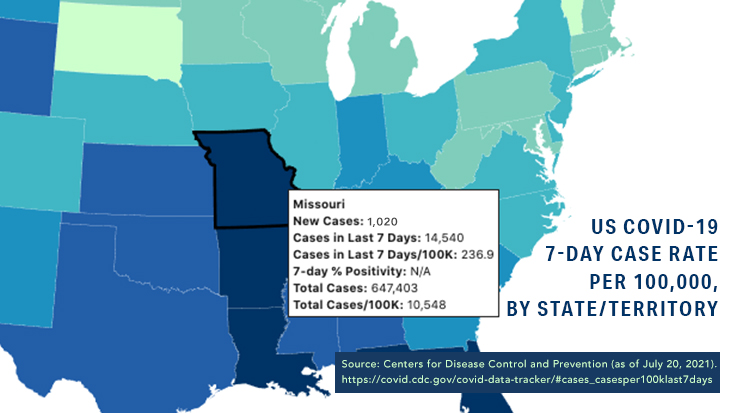
One such area is Southwest Missouri, where therapists are being pushed to their limits.
Record numbers of patients
“The surge has been very overwhelming for the medical resources in our community,” said Jonathan Brown, BSRC, RRT, RRT-ACCS, RRT-NPS, staff educator at Mercy Hospital in Springfield. “We are already seeing record numbers of COVID-19 patients in our census, and we anxiously anticipate that it may get worse following the Fourth of July holiday.”
He chalks the rise in new cases up to low vaccination rates and the Delta variant and believes increased summer tourism, fewer people wearing masks, and the abandonment of social distancing in many places are coming into play.
The patient population is getting younger too.
“In addition to the patients that we have always considered high risk, we are seeing many more young to middle-aged adults who were previously healthy,” Brown said.
He stresses that most of these patients are unvaccinated as well.
A colleague of Brown’s at another Mercy Hospital in nearby Joplin, also experiencing a surge, echoes that sentiment.
“Nearly all the patients in the ICUs have been unvaccinated, and of all the COVID-19 positive patients in the hospital, only approximately 10% have been fully vaccinated,” said Christopher Cox, clinical education manager, organizational effectiveness: talent development. “Vaccines appear to make a difference in the severity of illness and hospitalization.”
He notes that many large hospital systems in Missouri now require health care workers to be vaccinated to protect their patients and their fellow workers.
A cry for help
Brandon Burk, MS, RRT, RRT-ACCS, program director of the respiratory therapy program at Ozarks Technical Community College in Springfield, agrees it’s hard to pin the surge on just one factor. Still, like Brown, he thinks lack of vaccinations, the Delta variant, and the easing of preventative measures like mask-wearing and social distancing are the primary suspects.
“It has gotten much worse in the past few weeks,” he said. “In fact, we are experiencing a higher peak now than we did at the height of the pandemic in the winter, before vaccines were available.”
The local hospitals, he continues, are all overrun with patients, and he told us that just last week, one hospital CEO took to social media to beg all willing and able RTs to come and help. By the end of the day, 40 therapists had responded.
“Another hospital had to borrow ventilators from a sister hospital because they ran out, which was unprecedented in the history of the hospital,” he said. “Staff are working extra and are burnt out and dejected because they thought that the worst was over, but as we have seen, it is not.”
He says they are begging the community to step up and get vaccinated.
“They are being pushed past their breaking point,” Burk said. “They are still doing the best for their patients, but they are exhausted, both mentally and physically.”
They were ready
Despite the overwhelming amount of work facing RTs and their facilities, though, Jonathan Brown believes hospitals in Southwest Missouri were better prepared for this surge than they were for those that took place earlier in the pandemic.
“We already had policies and procedures in place this time, and we know more about COVID-19 now than we did at the beginning of the pandemic,” he said. “We have plenty of vaccines and PPE this time around, so that gives staff a lot more security.”
At Mercy, they have all the equipment they need too.
“We increased our fleet of high flow oxygen devices during the first surge, and it has become much easier to rent and borrow equipment,” he said.
It helps to be part of a big hospital system.
“Our organization has 30 acute care and critical access hospitals, and all the respiratory departments are collaborating to share equipment and supplies with the hospitals that need them most,” Brown said.
Brown says the most significant need at Mercy right now is staffing. With incredibly high workloads, it is becoming increasingly difficult to meet demand. Thankfully, they have been able to bring in contract workers to fill in some of the gaps. They have also recruited a significant number of new grads in the past few months.
“It has been all hands on deck for the last few weeks, with everyone, including clinical department leadership, taking care of patients,” he said.
Still, the surge is having an impact on the physical and mental health of staff.
“Many of us have had friends and family members who have died while fighting the virus,” Brown said. “Almost all our staff has taken care of patients who eventually died in our hospital while fighting the virus.”
Mercy has taken several steps to help. For example, the organization has a 24/7 phone number that workers can call to receive free counseling, and leaders have gone through additional training to develop resilience among staff. Several process improvement projects have also been initiated to make the therapist’s job easier.
Christopher Cox believes it is all having the intended effect.
“Despite the increased workloads, sicker patients, and donning the required PPE, RTs have shown incredible resilience,” he said.
Respiratory support is key
What have these therapists learned about treating patients with the more highly contagious Delta variant during the past few weeks of this latest surge? For the most part, it’s just more of the same.
“These patients don’t require different treatments,” Brown said. “We have just gotten better at providing treatments.” For example, he notes that staff didn’t have much experience with proning intubated patients before the pandemic and didn’t feel comfortable with the procedure. Now they have protocols in place.
“Our front-line staff has been driving most of the process improvement,” he continued. Improving communication between nurses and RTs has been paramount, as has developing ways to reduce pressure injuries.
Therapists at Mercy are also turning to CPAP, BiPAP, or the high flow nasal cannula to support patients before considering intubation, and if intubation cannot be avoided, they manage their ventilators with low tidal volumes and higher levels of PEEP.
They continuously nebulize Epoprostenol for refractory hypoxemia, and their physicians will typically order steroids and an antiviral medication as well and sometimes use convalescent plasma.
But Brown emphasizes the most important factor is providing respiratory support.
“Just like other causes of ARDS, all we can really do is support the patient until they recover and do the best that we can to prevent further damage to their lungs and other organs,” Brown said.
The one thing that is somewhat different this time is that ECMO is playing a more significant role, mainly because patients are younger and were otherwise healthy before they were struck with the virus.
“Mercy Hospital Springfield, in particular, has been experiencing better outcomes with ECMO patients during this surge compared to the last,” Brown said. “Part of that can be attributed to the patient population being much younger this time around, but we are also cannulating them sooner than we did previously.”
He believes early cannulation helps to mitigate some of the lung damage induced by the ventilator.
Keep your guard up
What advice do these RTs have for their fellow RTs who may be basking in the glow of plummeting COVID-19 cases right now?
Christopher Cox warns them not to let their guard down.
“RT leaders need to develop contingency plans for both noninvasive and invasive ventilation equipment,” he said. ”Find out what companies or hospitals are available to provide equipment when inventory is low.”
Brown says hospitals need to recognize their limitations too and plan accordingly. For example, many facilities lack an ECMO program. Waiting too long to transfer patients who could benefit from this treatment could be devastating.
And if you do have an ECMO program, plan to be busy because so many of the COVID-19 patients now are younger and will have a better chance with ECMO. That’s what’s happening at his hospital right now.
“Mercy Springfield is receiving a lot of transfers and consults right now due to a bigger patient population that is relatively younger with fewer comorbidities,” Brown said.
Cox also suggests hospitals take a careful look at staffing and develop creative plans to deal with the workload if all critical care beds are filled with ventilated patients. It’s essential to take a team approach as well.
“Make sure RTs are involved in leadership staffing plans and incident command planning,” he said. ”Ensure there is plenty of PPE equipment available. RTs provide life-saving skills when patients are often the most vulnerable. Use this as an opportunity to spotlight the clinical skills and support RTs can provide.”
Heroes, every one
These therapists stress that they are working 24/7 to ensure quality care for COVID-19 patients in their communities. But they would like to see people take advantage of the vaccines that are now readily available to prevent the disease. Or if they won’t, to realize that preventative measures like mask-wearing and social distancing need to remain their new normal.
“The only true treatment for any strain of COVID-19 is prevention,” Brown said. “There are many steps that people can take to protect themselves from exposure to the virus and help mitigate the risk of severe illness if you do get it. We urge people to take this virus seriously and follow the CDC guidelines to protect themselves.”
In the meantime, they send kudos out to their colleagues still battling COVID-19 on the front lines.
“We are so appreciative of all the respiratory therapists who don’t hesitate to provide life-saving care, even though their personal health may be at risk. You are all heroes,” Cox said.
Email newsroom@aarc.org with questions or comments, we’d love to hear from you.













