In July, a study published by the AARC’s science journal, Respiratory Care, reported results from a national survey of RTs aimed at gauging the prevalence of burnout among therapists amid the COVID-19 pandemic.
Conducted between January and March of this year, the poll showed 79% of respondents reported some level of burnout, with 10% reporting severe burnout.
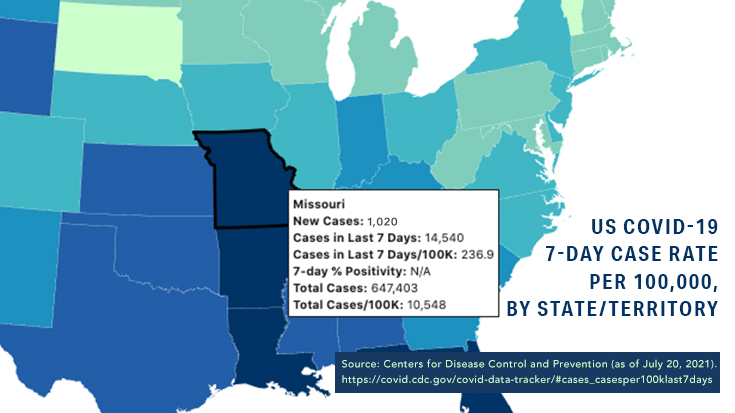
Now, here we are in late summer 2021, and the pandemic that first hit our shores in the winter of 2020 is still with us. The Delta variant has been a gamer changer, and is ripping through the country at breakneck speed.
How are therapists holding up? Two therapists share their experiences with burnout over these many months of COVID-19.
An emotional toll
“Like all members of the health care team, respiratory therapists have been greatly impacted by the COVID-19 pandemic,” said Jackie Williams, BS, RRT, a therapist at Salem Health, Hospitals & Clinics in Salem, OR. “It has caused an emotional toll on all RTs, from critical care to floor therapists to discharge planners.”
While she says morale was high at the beginning of the pandemic in her part of the country — everyone felt proud to be a part of the pandemic team and therapists were buoyed by all the positive press they were getting for their role — as the months have marched on and wave after wave has struck, therapists are feeling overwhelmed.
“We all had to adapt to the fact that things were only getting worse, not better, and that we were feeling more and more helpless when it came to caring for our patients,” she said. “We all have taken a second look at what matters most these days.”
For more than a few, that has meant dropping back to part-time or unscheduled to accommodate their family lives. Some therapists in her area have even retired from the profession completely. Staffing is short in almost all hospitals in Oregon now as a result.
“My hospital has 10 positions open currently, about 10% of our staff, including the manager,” she said. “We have hired more travelers than ever.”
Not being able to help their patients recover has been the worst part of the ordeal for many RTs.
“It goes against all of our caregiving nature to know that, no matter what we do, it’s not helping,” Williams said. Watching patients suffer alone in the ICU for a prolonged time has been the hardest thing she and her colleagues have faced.
The fact that so many people getting sick now are those who have refused vaccination is a bitter pill to swallow.
“RTs are angry at people who choose not to get vaccinated, knowingly placing us at risk in order to defend their own ‘rights’ or ‘opinions,’ which are usually uneducated,” she said.
Resiliency in action
As the RT director at Saline Memorial Hospital in Benton, AR, David Gibson, RRT, RRT-NPS, RPFT, TTS, has been in the thick of the latest COVID-19 wave this summer.
“We are seeing a surge, especially in the younger age group,” he said. “We are also seeing fully vaccinated patients on the ventilator.”
From a therapy standpoint, though, he and his RTs are better prepared than they were earlier in the pandemic.
“We know what to expect compared to when we started,” he said. “High flow therapy is key, as are the infusions.”
Gibson says his therapists are holding up fairly well.
“We have a strong group of RTs who utilize protocols and are very resilient,” he said. “The RTs are very dedicated and committed to their profession and providing excellent care at the bedside.”
But like his colleague up in Oregon, he admits some parts of the pandemic are still tough to deal with.
“The worst effects are witnessing the death of patients and the effects on their family,” Gibson said. “We are a close-knit community.”
Caring for the caregivers
Gibson has gone above and beyond to make sure his therapists receive the compassionate care they need to keep delivering compassionate care to their patients.
“We are being intentional about monitoring our RTs’ state of mind, trying to ensure we have adequate staffing and ensuring we keep a positive outlook,” he said.
He believes being open and honest with staff is the key — no spin talk allowed. They also celebrate their RTs and the students who rotate through their hospital and recognize all the hard work they are putting in to help the hospital deal with the crisis.
“Each day, we promote a positive work environment and remind ourselves that the only thing we can control today is our attitude,” Gibson said.
Keeping staff safe is job one. Gibson says they regularly discuss strategies to reduce contamination through filtered nebs, code blue processes, and other initiatives.
“From the beginning, we switched to filtered nebulizers or the Aeroeclipse nebulizers to prevent secondhand aerosol,” he said. “Anything and everything we can do to keep our staff safe is a key priority.”
Financial incentives are appreciated
Jackie Williams says her hospital stepped up to support its therapists with its pocketbook, and that has been appreciated.
“At the beginning, the hospital was offering all kinds of overtime shifts even when staffing was fine so that we could brush up on skills, training non-RT staff on intubations and ventilators, and cross-training on new equipment,” she said.
Those initiatives, plus all the positive press and kudos from the community showered on RTs early on, kept burnout at bay for a while. But as the pandemic dragged on, burnout happened anyway, and some therapists are severely affected.
The hospital is now playing catch up, once again offering financial incentives, like extra pay on top of overtime, PTO bonus time, and even a $1,000 thank-you check.
She believes the financial strategies have paid off the most for her facility.
“I believe that the initial unrestricted overtime offered and value that was placed on the staff as essential workers helped us all to want to work hard as a team to get through this hard time,” she said. In addition, giving therapists the tools they needed at the time made them feel like they truly mattered.
“When RTs feel like a valuable part of the care team, they get involved, stay involved, and speak up,” continued Williams. “The $1,000 bonus was also a nice gift.”
Little things work wonders
Gibson believes his staff has weathered the COVID-19 storm as well as they have in part because his department puts a great emphasis on a positive attitude when they hire new RTs. Listening to those therapists and addressing their concerns has made a world of difference too.
“Our RTs help identify opportunities for improvement,” he said. “Creating an environment which respects everyone’s opinions is key.”
But sometimes, the little things can work wonders too.
At his hospital, that benefit comes in the form of a daily “recess,” giving staff time together to relax and brush up on their communication skills at the same time.
“We play a simple game that allows us to take a break from the hectic environment,” Gibson said.
The game is called Catchphrase and requires players to communicate with their teammates to succeed.
“This means we have to be intentional about what the other person is saying and how they are saying it,” he said.
Taking a breather to play a game could never replace the more concrete steps Gibson’s department has taken to mitigate the effects of burnout. Still, it shows staff that their leaders care enough to interject some fun and distraction into what are often long and trying days.
These days, RT departments can use all the fun and distraction they can get.
Email newsroom@aarc.org with questions or comments, we’d love to hear from you.