COVID-19 has impacted just about every hospital in the country, and many are still battling the virus today. But everyone involved in the care of COVID-19 patients is a lot wiser now than they were in the beginning. For example, respiratory therapists at Temple Health in Philadelphia, PA, believe the measures they took and the lessons they learned early on went a long way toward ensuring the best possible outcomes for their patients.
The early days
Associated with Temple University, Temple Health can trace its roots back to the founding of 20-bed Samaritan Hospital in 1892 by Temple University president Dr. Russell Conwell. Its key mission was to provide free care for those unable to afford payment, regardless of race, nationality, or creed.
 Hernan Alvarado led the way for RTs at Temple during the COVID-19 crisis.
Hernan Alvarado led the way for RTs at Temple during the COVID-19 crisis. Today the system consists of three hospitals and a major cancer center, along with multiple other facilities. Together they account for more than 1,000 licensed beds and employ over 10,000 faculty members and employees. Hernan Alvarado, Jr., MBA, RRT, RPFT, is associate vice president for respiratory care and sleep diagnostics services.
He recalls the system’s introduction to COVID-19 in the spring of 2020.
“Beginning of March, we started to see the impact of COVID hospitalization,” he said. “We increased our inventory and secured supplies for about three months and continued to replenish the stockpile.”
They decided to isolate COVID-19 patients to one tower in the hospital. The respiratory therapy department recruited volunteers to support the building. They opened schedules to ensure they could meet patient needs. They canceled penalties for late arrivals to facilitate the frequent switches between staff that were deemed necessary.
Their mechanical support capability tripled with the addition of ventilators, high flow nasal cannulas (HFNC), and BIPAP machines.
Innovative care

By April, the hospital was at total capacity, and patient surges pushed the facility to double up rooms. That continued into the second wave of the virus. Respiratory therapists were there to provide the full support these patients needed.
Thoughtful decisions were made as to what that support would entail.
“When hospitals across the U.S. went to mechanical vents, HME, and MDI, Temple continued our standard of care with heater humidification systems and administered nebulizer treatments,” Alvarado said. “We primarily used HFNC and BIPAP as the standard of care and escalated to mechanical vent as we usually do with a respiratory infection.”
They also enrolled their COVID patients in investigational drug studies, which gave most of them the extra support they needed to get through their bout with the infection. Alvarado says their chief of pulmonary medicine, Gerard Criner, MD, also held daily Zoom or Teams calls with therapists to review international, national, and local updates on the pandemic.
“We reviewed vent and RT capacity, medication delivery, weaning approaches, and opened it up to discussion,” he said.
RTs deemed essential

Dr. Criner says RTs were essential in treating COVID-19 patients from the beginning of the pandemic onward.
“Respiratory has been at the front lines of securing equipment and having in place essential elements for noninvasive oxygenation and ventilatory support, included high flow nasal therapy and noninvasive ventilation and use of nebulized Flolan,” he said.
“In fact,” added the physician, “the first reported use of high flow nasal therapy in COVID-19 pneumonia was published based on the work of our RT department.”
He also credits the department with securing the necessary ventilators and creating ventilator surrogates if the hospital became overwhelmed by a lack of invasive ventilator units. Fortunately, that didn’t happen — the department’s use of other strategies warded off a worst-case scenario.
“Due to their dedication and hard work and expertise in the use of noninvasive sources of oxygenation and ventilation, we never exceeded 14% of our COVID population that needed invasive ventilation, even during the height of the pandemic,” Dr. Criner said.
Balancing act
Alvarado says managing the equipment part of the equation for all the hospitals in the system was a balancing act.
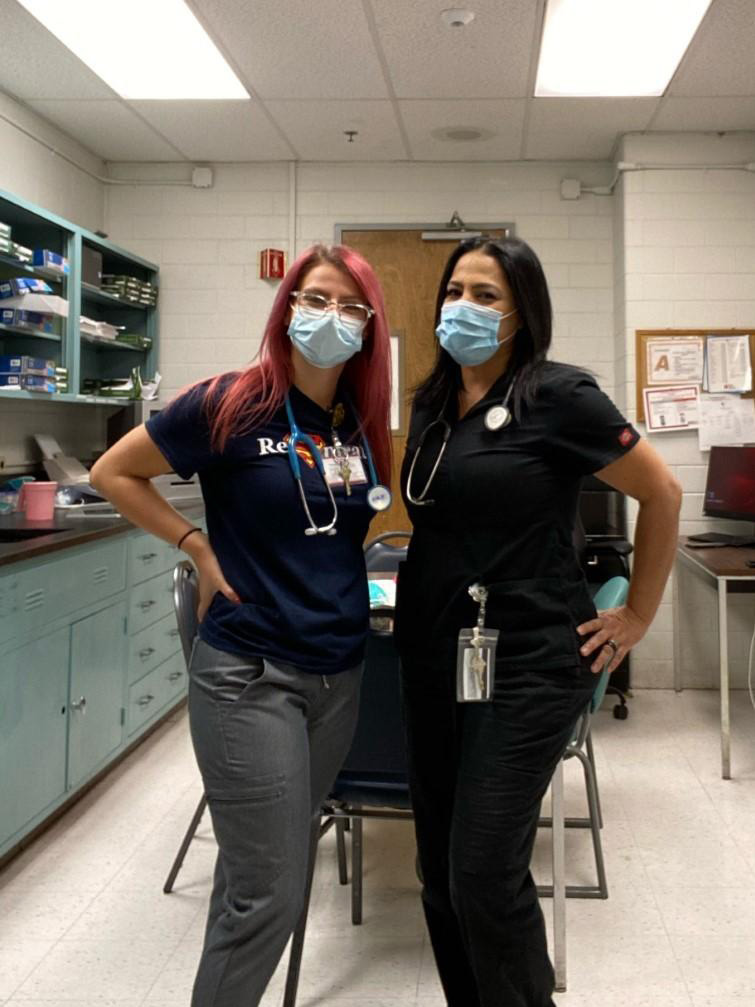 These are just some of the Temple RTs who kept respiratory care running smoothly during COVID-19.
These are just some of the Temple RTs who kept respiratory care running smoothly during COVID-19. “As the lead for respiratory care in the health system, I instituted an inventory spreadsheet that allowed for the most up-to-date inventory on ventilators, NIV, high flow nasal cannula,” he said. “This allowed us to shift resources when needed.”
Filters and other disposables were shared between the facilities because one facility often would have been able to secure supplies while another was hurting for inventory.
“This allowed us to think as one large RT department and not individual campuses,” Alvarado said.
In all events, the overriding goal was to ensure that the most severe cases received the highest level of ventilator available.
Maintaining services

In the early months of the pandemic, many hospitals completely shut down their pulmonary function laboratories and other respiratory-related services. Alvarado says that never happened at Temple. Instead, while working overtime to manage the COVID-19 crisis, they made a conscious decision to keep both their pulmonary diagnostics and sleep services up and running.
COVID-19 guidelines established by Temple medical directors, infection control experts, and departmental subject matter experts, along with CDC recommendations, were instituted for pulmonary function testing and bronchoscopy. As part of the process, bronchoscopy switched to disposable bronchs typically used in the critical care units and maintained full PPE and minimal staffing.
Alvarado says the bronch procedures would ideally be for non-COVID-19 patients, but they decided not to limit them entirely if they used the correct environment and PPE.
In the PFT lab, flow sensors were changed between patients, and rooms were alternated. The lab ceased using nebulization with conversion to MDIs, and instituted a reduction in the testing offered. Specifically, methacholine challenges were curtailed. In addition, full PPE was required for staff.
On the sleep side, they pivoted from largely in-person testing to more home sleep testing (HST). They reviewed their inventory to ensure disposable products were used whenever possible and examined their processing procedures for non-disposable components. Complete disposable HST kits were sent directly to the patients’ homes, and telemed visits allowed the patients to be seen by a clinician.
Staff offered inpatient sleep studies on a limited basis.
“We maintained operations by implementing COVID guidelines that entailed COVID testing within 48-72 hours prior, N-95s, and appropriate PPE for sleep techs and alternating rooms to allow air exchanges,” Alvarado said. “Our staff was screened upon entrance to the campus and department.”
Recipe for success
Hernan Alvarado says he learned several valuable lessons during the initial phases of the COVID-19 pandemic that have served his hospitals well. First and foremost, to manage COVID-19 patients without limitations or fears. By that, he means “delivering care in a safe, effective manner by instituting guidelines to limit exposure but not limit the aggressiveness of bronchopulmonary care.”
He also believes his health system benefited greatly from system integration — the idea that all the hospitals in the system could support each other throughout the crisis. And he cites Temple’s conversion of non-clinical areas into acceptable clinical spaces for expanding their outreach capabilities.
Throughout it all, his RTs were there to ensure the respiratory care patients received went as smoothly as possible.
Dr. Criner says those therapists were instrumental in all stages of the pandemic.
“I am proud and honored to be their colleague,” he said. “Their dedication and devotion to patient care at their own risk is admirable and an example for all of us.”
Email newsroom@aarc.org with questions or comments, we’d love to hear from you.