
The emergency department (ED) can be a wild place to work. There’s a reason there was a TV show called “ER,” not “Med-Surg” or “RT Department.” Full disclosure: I think a TV show about RTs would be pretty interesting, based on some of the characters I’ve met over the years. Nearly everyone who has been a respiratory therapist (RT) for a long time will be able to share at least a couple of unconventional, frequently disgusting, but always exciting stories from the ED. However, these stories result in a distorted view of what working in the ED is like, as even in the busiest EDs, stories like these are rare occurrences. Most of the work done by RTs in the ED is standard work, like delivering inhaled medications, managing mechanical ventilation, patient assessment, and airway management. An ED RT needs to be able to adapt to rapidly changing acuity and unexpected patient arrivals while dealing with a wide variety of patient populations.
Essential Skills for Emergency Department RTs
RTs in the ED will encounter every type of patient, from newborns to elderly nursing home patients and anything in between, often within a single shift. Patients present to the ED with undifferentiated respiratory distress. It can be challenging to determine the underlying pathophysiology to initiate the best treatment. In most critical cases, the only history will be from emergency medical service providers, who have limited time to get a medical history from family or the patient and in many patients, it will not be possible to get a medical history at all. In these cases, the team’s ability to rapidly assess the patient to initiate the correct treatment.
The foundation for success for RTs in the ED is strong patient assessment skills and an understanding of the pathophysiology of various disorders. RTs should know how to assess neonates, children, and adults. In our facility, RTs working in the ED complete NRP, PALS, and ACLS. While these courses do not provide all the skills necessary to succeed in the ED, they offer a solid foundation for building additional skills. Some departments may also require or highly encourage advanced trauma life support for those staffing in the ED. Recognizing the cause of illness and initiating the correct treatment is something RTs do not regularly apply but RTs expertise and assessment skills can help physicians make diagnoses. Most inpatients have already received a diagnosis and have a complete history available. Many hospitals have RT-driven protocols in place without the need for a physician to evaluate a patient. These protocols may include initiating bronchodilator therapy, noninvasive ventilation, or drawing arterial blood gases. In busy EDs, RTs may assist in triage to help nursing evaluate if patients with respiratory disorders need immediate treatment or if they are stable enough to remain in the waiting room. RTs working in the ED will need to have a working knowledge of ED triage systems.1 The decision to admit patients to the ICU or general wards may also be influenced by the RT, especially for those patients requiring increased respiratory support.
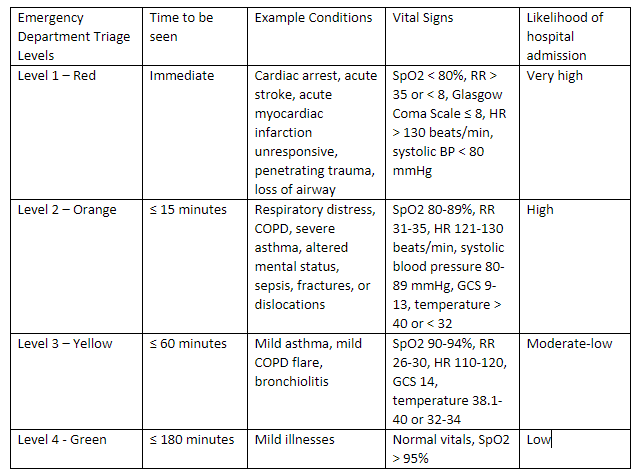
Adapted from: Barfod C, Lauritzen MM, Danker JK, Soletormos G, Forberg JL, Berlac PA, et al. Abnormal vital signs are strong predictors for intensive care unit admission and in-hospital mortality in adults triaged in the emergency department – a prospective cohort study. Scand J Trauma Resusc Emerg Med 2012;20:28.
In addition to assessment skills, RTs working in the ED will need strong airway management skills, including manual ventilation, airway adjuncts, tracheostomy troubleshooting, and endotracheal intubation. RTs are the experts in managing tracheostomy patients within the ED, able to identify common tracheostomy-related issues. A common procedure in the ED, endotracheal intubation is often performed under suboptimal conditions due to physiologic, anatomic, or external challenges such as cervical spine collars in trauma patients. RTs must understand various methods of intubation used, such as direct laryngoscopy and video laryngoscopy.2,3 Other procedures could include arterial line placement4,5,6, placing intravenous catheters, naso/orogastric tubes, lung ultrasound7, or placing central lines.8 Generally, if RTs are licensed to place arterial lines, they are also credentialed to place IVs, although RTs scope of practice varies from state to state and center to center.4 The frequency and type of top-of-the-license RT procedures depend upon local needs and the availability of RTs to perform the task.
High-Value Care RTs can provide in the ED
Procedures
- Intubation
- Arterial line placement
- Central line placement
Protocols
- Invasive mechanical ventilation
- Noninvasive mechanical ventilation
- High-flow nasal cannula
- Asthma
- Bronchiolitis
Patient Education
- Medication teaching
- Smoking cessation
Perhaps the most significant value of having RTs in the ED is noninvasive and invasive mechanical ventilation management. Despite solid evidence of its effectiveness, lung-protective ventilation is underused in both adults and children with ARDS.9,10 In the ED, implementation of lung-protective ventilation has been associated with improved mortality, increase in ventilator-free days, and development of ARDS.11,12 In our facility, all patients receiving mechanical ventilation are managed via the same RT driven, lung-protective protocol. NIV is widely applied in the ED for various indications and proves to improve mortality in both COPD and cardiogenic pulmonary edema.13 In addition to accepted indications, NIV may be used in de novo respiratory failure, trauma, asthma, and ARDS, although the utility in these disease states is unclear.14 An important aspect for patients requiring NIV is that the optimal timing of intubation is unclear, and an experienced RT can help guide ED physicians. The technical knowledge possessed by RTs can help optimize aerosol delivery for patients with COPD or asthma exacerbations during NIV.15 Similar to invasive ventilation, RT-driven protocol also drives NIV within our facility. High-flow nasal cannula use has also dramatically increased in the past decade, and RTs can help guide physicians on when to initiate NIV vs. HFNC. Protocols should be developed to give RTs autonomy and incorporate the most recent evidence to provide patients with the best treatment possible.13
Lastly, RTs will provide patient education for those presenting with respiratory disorders. Unfortunately, the ED is often the only point some people interact with the health care system. The ED RT can take the opportunity to ensure patients know how to use their medications correctly, understand when, why, and how to take their inhalers, recognize symptoms of respiratory difficulty, and identify patients who may need help to get access to their medications. Properly educating a patient can help reduce their likelihood of returning to the ED while improving their overall quality of life. An example would be to recommend an inhaled corticosteroid for a patient with asthma who frequently comes to the ED for care but does not have a primary care physician.16 RTs staffing the ED should consider obtaining the AE-C certification from the National Asthma Certification Board to help optimize outcome for asthma patients within the ED.5
What it Takes
Success in the ED is challenging to quantify because it requires RTs to adapt to rapidly changing conditions. Every day is a new challenge with all new patients. A wise mentor once told me that the ED is hours of boredom interrupted by minutes of sheer terror. Activity can go from mundane nebulizer treatments in patients with low acuity, to instant chaos with multiple traumas requiring intubation and CT scans or critically ill patients requiring NIV. The uncontrolled circumstances of the ED can be overwhelming for RTs who are accustomed to being able to plan their day carefully. When it’s hectic, specific tasks may need to be done more quickly than usual or delegated to another RT or RN. These competing priorities alone make it a stressful environment. Paired with frequent exposure to unexpected deaths from accidents or other causes can make the ED a challenging climate emotionally, even for the most seasoned RT.
The ideal clinical skills needed to work successfully in the ED include, but are not limited to, the ability to adapt, and the resilience to bounce back after rough shifts or tragic cases. In addition, they need to be a strong communicator and be willing to make decisions with incomplete information. Specific cases such as sudden infant death syndrome, pediatric trauma, and unexpected death of young people are particularly challenging if one is unprepared. ED therapists also need to be team players often pitching in when multiple hands are needed. It may be unavoidable to assist with combative trauma patients, patients with psychiatric disorders, setting up hemodynamic monitoring equipment, assist with line placement, or do ECGs; tasks that are within the scope of RT practice, but not particularly common place in all institutions. In teaching hospitals, RTs will also help educate resident physicians and nurses about the mechanical ventilation and other aspects of respiratory care.
Future Role of RTs in the ED
While RTs currently have a significant impact in the ED, the increased use of RT protocols will demonstrate RTs’ value in the future. An important area of future research is hospital admission and outcomes for patients treated by RT protocol in the ED. Smoking cessation and patient education are other areas where future research is needed.
References
- Barfod C, Lauritzen MM, Danker JK, Soletormos G, Forberg JL, Berlac PA, et al. Abnormal vital signs are strong predictors for intensive care unit admission and in-hospital mortality in adults triaged in the emergency department – a prospective cohort study. Scand J Trauma Resusc Emerg Med 2012;20:28.
- Miller AG. Endotracheal Intubation Training and Skill Maintenance for Respiratory Therapists. Respir Care 2017;62(2):156-162.
- Miller AG, Gentile MA, Coyle JP. Respiratory Therapist Endotracheal Intubation Practices. Respir Care 2020;65(7):954-960.
- Miller AG, Cappiello JL, Gentile MA, Almond AM, Thalman JJ, MacIntyre NR. Analysis of radial artery catheter placement by respiratory therapists using ultrasound guidance. Respir Care 2014;59(12):1813-1816.
- Rowley DD, Mayo DF, Durbin CG, Jr. Initial experience with a respiratory therapist arterial line placement service. Respir Care 2000;45(5):482-485.
- Pack S, Hahn PY, Stoller JK, Mummadi SR. Respiratory Therapist-Managed Arterial Catheter Insertion and Maintenance Program: Experience in a Non-Teaching Community Hospital. Respir Care 2017;62(12):1520-1524.
- Karthika M, Wong D, Nair SG, Pillai LV, Mathew CS. Lung Ultrasound: The Emerging Role of Respiratory Therapists. Respir Care 2019;64(2):217-229.
- Ramirez C, Malloch K, Agee C. Evaluation of Respiratory Care Practitioner Central Venous Catheter Insertion Program. Journal of the Association for Vascular Access 2011;15(4):207-211.
- Khemani RG, Smith L, Lopez-Fernandez YM, Kwok J, Morzov R, Klein MJ, et al. Paediatric acute respiratory distress syndrome incidence and epidemiology (PARDIE): an international, observational study. Lancet Respir Med 2019;7(2):115-128.
- Bellani G, Laffey JG, Pham T, Fan E, Brochard L, Esteban A, et al. Epidemiology, Patterns of Care, and Mortality for Patients With Acute Respiratory Distress Syndrome in Intensive Care Units in 50 Countries. JAMA 2016;315(8):788-800.
- Fuller BM, Ferguson IT, Mohr NM, Drewry AM, Palmer C, Wessman BT, et al. Lung-Protective Ventilation Initiated in the Emergency Department (LOV-ED): A Quasi-Experimental, Before-After Trial. Ann Emerg Med 2017;70(3):406-418 e404.
- Fernando SM, Fan E, Rochwerg B, Burns KEA, Brochard LJ, Cook DJ, et al. Lung-Protective Ventilation and Associated Outcomes and Costs Among Patients Receiving Invasive Mechanical Ventilation in the ED. Chest 2021;159(2):606-618.
- Hess DR. Evidence-Based Respiratory Care. Respir Care 2021;66(7):1105-1119.
- Piraino T. Noninvasive Respiratory Support. Respir Care 2021;66(7):1128-1135.
- Hess DR. Aerosol Therapy During Noninvasive Ventilation or High-Flow Nasal Cannula. Respir Care 2015;60(6):880-891; discussion 891-883.
- Farmer A, Mirea L, Carter J, Rank M, Bulloch B, Vaidya V, et al. Inhaled corticosteroids prescriptions increased in the ED for recurrent asthma exacerbations by automated electronic reminders in the ED. J Asthma 2020;57(10):1140-1144.
Email newsroom@aarc.org with questions or comments, we’d love to hear from you.
















