
Higher Anticoagulation Dose May Reduce Mortality, Intubation
Results from the large-scale FREEDOM trial led by investigators from Mount Sinai Hospital suggest that the standard treatment with low-dose anticoagulants for patients with COVID-19 who are not considered severe should be changed to high-dose anticoagulants.
The study was conducted among 3,398 adults in 76 urban and rural hospitals across ten countries, including the U.S, who were hospitalized with confirmed COVID-19 but were not in the ICU or intubated. About half had signs of ARDS. Patients were randomized to prophylactic subcutaneous enoxaparin, therapeutic subcutaneous enoxaparin, or therapeutic oral apixaban within 24-48 hours of being admitted and followed for 30 days.
The combined therapeutic groups were compared to the prophylactic group. Among the findings –
- The primary endpoint of a combination of death, requirement for ICU care, systemic thromboembolism, or ischemic stroke at 30 days was not significantly reduced between the groups.
- 7% of patients treated with the prophylactic anticoagulation died within 30 days compared with 4.9% of patients treated with therapeutic anticoagulation, for an overall reduction of 30%.
- 6.4% of patients on the therapeutic regimen were intubated within 30 days compared with 8.4% in the prophylactic group, a 25% reduction.
- Among patients with ARDS at the time of hospital admission, 12.3% in the prophylactic anticoagulation group died within 30 days compared with 7.9% in the therapeutic anticoagulation group.
- All groups had low bleeding rates, and no differences were seen between the two therapeutic blood thinners for safety and efficacy.
“What we learned from this trial is that many patients hospitalized with COVID-19 with pulmonary involvement, but not yet in the intensive care unit, will benefit from high-dose subcutaneous enoxaparin or oral apixaban to inhibit thrombosis and the progression of the disease,” said lead author Valentin Fuster, MD, PhD. “This is the first study to show that high-dose anticoagulation may improve survival in this patient population — a major finding since COVID-19 deaths are still prevalent.”
The study was published by the Journal of the American College of Cardiology. Read More
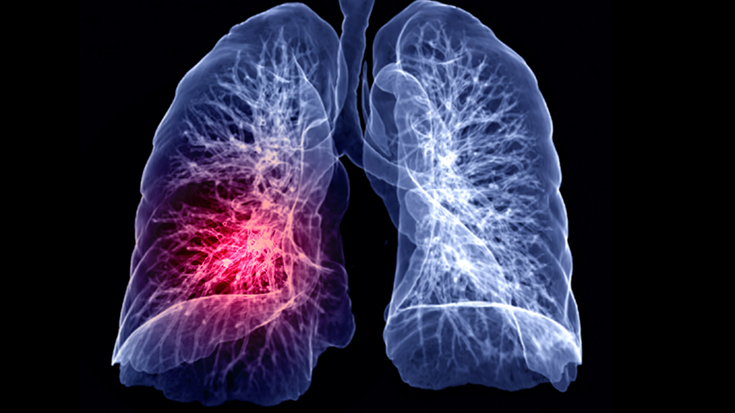
Lung Inflammation Study Gets Underway
Investigators from the University of Illinois Chicago have received a $13 million Program Project Grant from the National Heart, Lung and Blood Institute to study how the human immune system is regulated by the endothelium in lung tissue.
The work is expected to lead to new treatments for patients suffering from lung diseases like COPD, pulmonary fibrosis, and even ARDS.
“It is now becoming increasingly clear that the lung endothelium is a complex monolayer, an organ itself,” said Dolly Mehta, program director for the grant. “Studying this enigmatic immune regulatory function of lung endothelium is crucial for understanding how endothelial cells control immunity and defensive function of the lungs.”
The research will consist of three projects. One will look at a protein receptor in endothelial cells that promotes lung integrity, another will examine an enzyme called E3 ligase that influences the integrity of the lining of the blood vessels and the genes that activate the enzyme, and another will assess how mitochondria in endothelial cells can be leveraged to prevent out-of-control inflammation.
The researchers believe these cellular processes are interconnected and they hope to create an infrastructure for collaboration among those studying the various mechanisms involved. Read More

Early Life Factors Play a Role in Lung Health
New results from a British study that has been following 7,545 pregnant women and their children since 1991 to see what effect 33 different factors might have on the lung health of the children as they got older has identified six factors associated with lung health.
The researchers found that women with a higher body mass index during pregnancy and those who smoked while pregnant were more likely to have children who grew up to have lower lung function. Children with a lower birth weight, those with a higher fat mass or lower lean mass when they started primary school, and those with early-onset asthma were more likely to have poorer lung function at age 24 as well.
“Compared to previous studies on lung health, our work stands out as being the most comprehensive of its kind, to date, as it considers the underlying relationships between these 33 factors, offering reliable findings on their importance on adulthood lung health,” said lead researcher Dr. Osama Mahmoud, from the University of Essex.
The investigators believe the factors they identified in their study can be used to develop predictive tools for respiratory health and reduce health care inequality by targeting early-life interventions.
The study was published by the European Respiratory Journal. Read More
Email newsroom@aarc.org with questions or comments, we’d love to hear from you.













