A recent study conducted in a large hospital system in Arizona found an inhaler to nebulization protocol saved the system more than $1.5 million over the first year of operation without adversely impacting either length of stay or 30 day readmissions rates.
AARC members who have implemented these protocols in their facilities believe it’s the way to go too.
Two main goals
“St. Luke’s Health System in Boise converted to an inhaler to neb protocol in August of 2018,” said Dave Shuldes, RRT, who serves as respiratory therapy manager at the Idaho facility. “Pharmacy made the initial suggestion for the protocol. The details of the implementation process were a collaborative effort between Pharmacy and RT.”
Shuldes says the team established two main goals for the program.
- First, they wanted to create increased opportunity for therapists to be involved in patient education with all inhaled medication delivery — prior to the protocol, RNs were delivering many of the MDI doses.
- Second, they wanted to decrease MDI expense.
“We also knew a tertiary benefit would be improvement in RT productivity against benchmarks because these RT services are billable,” he said.
In his hospital, all patients with inhaled medication orders come under the protocol.
“RT now delivers 100% of inhaled med doses and seeks opportunity for patient/family education with all treatments,” he said.
The protocol has significantly increased the workload associated with medication delivery. That increase has been offset to some extent by a corresponding move to discontinue direct RT involvement with incentive spirometry, which Shuldes notes is a non-billable expense.
Cost savings have been substantial.
“The health system has saved more than $750K in MDI purchase expenses in the first year,” he says. “The RT department also has a better margin to support our work. We have improved our productivity position against benchmarks by almost 30%. This has had the tangible benefit of approval for requested positions.”
Feedback from staff members has been positive overall, and patients are on board too. Shuldes says their Press Ganey Top Box score on the question, “Understood purpose of taking meds” improved 12.3% in the year since the protocol was implemented.
“To put the improvement in context, we are now performing better than 99% of large hospitals and 97% of Magnet hospitals in the Press Ganey database on this question,” he said.
Critical access hospital
The inhaler to nebulization protocol at Trego County Lemke Memorial Hospital in Wakeeney, KS, was implemented primarily to save on costs, says Marlyce Campbell, CRT, director of respiratory care and the sleep lab.
“At our critical access hospital, it’s too expensive to do inhalers, and 98% of the patients didn’t know how to use them properly,” she said. “I had pharmacy put into the orders that if they ordered an MDI it would popup the nebulizer preferred meds.”
Respiratory therapists perform treatments and provide the patient education needed to ensure patients understand what they are getting and why. Many patients are happy to know the nebulizer option exists because it is significantly more cost effective for them as well.
“We have found out most patients can’t afford their inhalers, and most can get the neb meds covered for free,” Campbell said. The protocol hasn’t really affected the RT workload in her small facility.
Patients who do want to use inhalers benefit from instruction into their proper use, and they often express their gratitude for the education they received from the RTs.
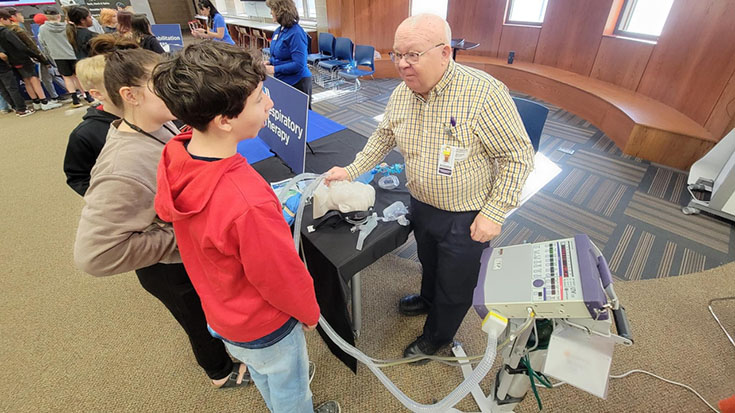
“We also have a machine that shows the patient if they are doing the technique correctly,” Campbell said. “It has helped a lot for the patient and the therapist.”
Productivity boost
At St. Mark’s Hospital in Salt Lake City, UT, Jack Fried, MS, BSRC, RRT, and his department have worked under an inhaler to neb protocol for several years now. Pharmacy drove the change, holding meetings with the people who would be involved on both shifts.
Most of the patients affected by the change are surgical patients with preexisting pulmonary diseases.
“We also have a few on our behavioral health and inpatient acute rehab units,” Fried said.
Despite some dire predictions prior to implementation of the protocol, workload has not really been affected.
“Initially, we had a few doomsday seers predict we’d be swamped with large numbers of additional treatments,” he said. “If anything, it has helped productivity during periods of low volume.”
Savings from the protocol came in at $60,000 for the first seven months and now exceed $100,000 per year, continued Fried.
No effect has been seen on patient outcomes.
“Some patients prefer to use their own inhalers, and we go through the hospital procedure of pharmacy labeling the inhalers and nurses scanning them at the appropriate administration times,” he said. “Other patients like the therapists’ visits, along with the opportunity to ask questions.”
Managers speak
Would these managers recommend an inhaler to nebulization protocol to their fellow RTs? In their own words —
Dave Shuldes: Absolutely yes. I encourage everyone considering this change to focus on the positive aspects of what your service is creating rather than what is “ending or being stopped.” It was easy for us to get caught up in imagining unhappy patients, unhappy providers, and overworked RTs. In the reality of our experience, decreased MDI costs has actually meant better care. There were many difficult issues addressed by the Pharmacy and RT along the way and change was difficult, but the benefits have clearly been worth the effort.
Marlyce Campbell: Yes. We are spending more time with the patients that really need us the most. We, as therapists, give therapy; nursing gives meds.
Jack Fried: I definitely recommend the conversion. It saves money, provides teaching moments, and improves productivity. The latter can be especially important in facilities similar to this one, where therapist-driven protocols mandated by our corporate office will likely continue the decrease in treatments.
Keep the conversation going
Share your thoughts and experiences with this topic on AARConnect. See what your colleagues have to say!
Email newsroom@aarc.org with questions or comments, we’d love to hear from you.