Regular competency assessments are a fact of life in a profession like respiratory care where facilities must ensure the ongoing ability of clinicians to deliver high-quality care. No one looks forward to them, but believe it or not, the managers and clinical educators charged with planning these activities really do work hard to make them not only meaningful, but enjoyable and – dare we say it? – fun at the same time.
3G simulations
Heather VanHorn, RRT, RRT-NPS, is director of respiratory care, electrocardiology, neurodiagnostic, and rehab services at Dignity Health in Redding, CA. She assesses competency in her staff through a skills fair using 3G simulation and a variety of scenarios tailored to the experience levels and expectations of the therapists taking part. It’s a strategy she believes helps to keep everyone engaged.
Hands-on demonstrations of skills mixed with information sharing and team building exercises in small group settings is another tactic that’s worked well in her department, and she also tries to make sure her RTs go well beyond the mere performance of a skill.
“My team leads do bedside competency check-off/real-time remediation,” VanHorn said. “This allows them to address the ‘why’ as well as the ‘how’ in a meaningful, educational interaction.”
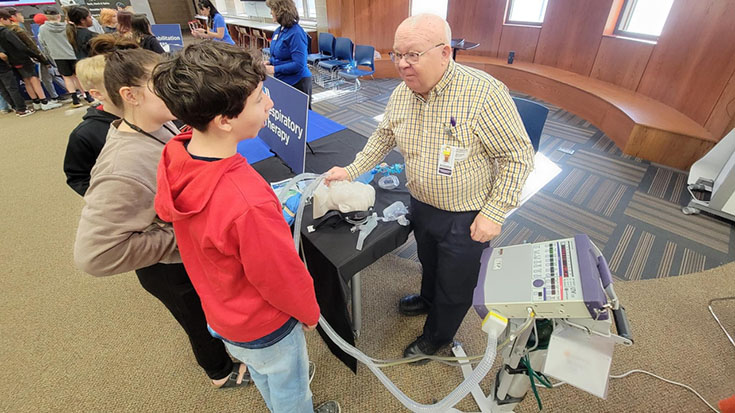
At the Children’s Hospital of Wisconsin in Milwaukee, Deb Bakalarski, RRT, respiratory care services scheduler and credentialed trainer-CHW EPIC, says they hold a four-hour competency day on an annual basis where RTs attend one hour of lecture, then break up into groups of 3-4 each to cycle through 3-4 mini practice scenarios, equipment setups, and question/answer sessions.
The competency day also includes a simulation in the hospital’s simulation lab that she says includes “things to do, things to answer, things to look at.”
Dividing RTs up into the small groups makes the competency day less intimidating and she even brings in breakfast and a mini-snack to ensure everyone is well nourished for the education to come.
“They do get paid for the four hours as well,” Bakalarski said.
Laugh and learn
Kathy Kammeraad, RRT, who works in clinical informatics for respiratory care at Spectrum Health in Grand Rapids, MI, finds special treats go a long way toward easing the pain of competency assessments as well.
“If the education is simple and only requires a flyer or feedback, I call it a ‘laugh and learn’ and staple a Laffy Taffy to the sheet,” she said. “My other go-to is to stock up on ‘Thank You’ Girl Scout cookies. They are great for recognition and as a treat for attending an in-service — especially when you pull them out post-Girl Scout cookie season.”
She believes educators can interject other types of fun into these sessions too.
“I just attended an event where they asked the participants to write their ideas/questions on paper airplanes and fly them to the front of the room — or wad them up and throw them,” Kammeraad said.
Being considerate of staff time can help make competency assessments more tenable for staff too, says Shawna Murray, MEd, RRT, system learning business partner for respiratory, sleep medicine, pain services, wound care, and hyperbaric medicine at Intermountain Healthcare in Salt Lake City, UT, particularly when they are held outside of working hours.
“One option is to hold ‘skills stations’ before and after shift change during a week-long time period and allow staff to stop by the skills station at any time during that week-long time period,” she said. “All information related to the skill — i.e. policies, procedures, protocols, manufacturers’ information, etc. — should be made available two weeks ahead of time, allowing staff to review the information they’ll need to demonstrate competency.”
She also believes that scenario-based assessments, return demonstrations or skill pass-offs for pieces of equipment, and quizzes can figure into successful competency assessments. In cases where the information will need to be verified by a surveyor or other entity, she suggests using a read/response method, or posting the document on a shared data source like Office 365 and having people “like” the document after they read it.
The one thing she doesn’t believe should be included in competency assessments is competition.
“Creating competition in the department by regularly scheduling assessments in any form and posting the scores can be detrimental, even if the intent was to have some ‘fun,’” Murray said. “Assessing and labeling an individual as ‘competent’ or ‘less than competent’ — either directly or indirectly — can have unintended impacts on career advancements, morale, and ultimately legal action.”
Give it a chance!
The next time you’re scheduled for a competency assessment, forego the normal urge to groan and instead find a way to look forward to the opportunity. Your managers and educators put a lot of time and effort into these sessions and you never know what they may have in store!
Email newsroom@aarc.org with questions or comments, we’d love to hear from you.