It’s in the Air, but is it Infectious?

New research in JAMA Network Open provides some perspective on just how dangerous the air in hospitals has become during the COVID-19 pandemic.
The European investigators searched the medical literature for studies on air contamination with SARS-CoV-2 in hospital settings published between Jan. 1 and Oct. 27, 2020. Twenty-four studies met their criteria. Overall, 17.4% of 471 air samples taken from close patient environments were positive for SARS-CoV-2 RNA. Samples taken from the ICU were significantly more likely to be positive than those taken from non-ICU areas. Distance from patients did not affect the findings. The positivity rate in toilets was 23.8%, in clinical areas 8.3%, in staff areas 12.3%, and public areas 33.3%.
Despite the air contamination found in these studies, however, viral cultures performed in five trials found only 8.6% of 81 samples tested were positive for viable virus. All of these were taken from close patient environments. Still, the authors believe the high viral loads seen in toilets and bathrooms, staff areas, and public hallways deserve more attention.
Substances in Meat Linked to Childhood Wheeze

Children with asthma may wheeze more if they eat more cooked meats, report researchers from Mount Sinai in New York City who used data from the 2003-2006 National Health and Nutrition Examination Survey to look at the link between substances in meat called advanced glycation end-products (AGEs) and childhood wheeze.
The study, published in Thorax involved 4,388 kids between the ages of two and 17 and evaluated the association between dietary AGE, meat consumption, and respiratory symptoms. Results showed higher AGE intake increased the odds of wheezing, particularly wheezing that disrupted sleep and exercise. Kids with a higher intake of non-seafood meat were also more likely to have sleep and exercise wheezing that required treatment with prescription medication. The findings held despite the overall quality of the child’s diet.
“Research identifying dietary factors that influence respiratory symptoms in children is important, as these risks are potentially modifiable and can help guide health recommendations,” said senior study author Sonali Bose. “Our findings will hopefully inform future longitudinal studies to further investigate whether these specific dietary components play a role in childhood airways disease such as asthma.”
Lung Cancer Screening in the Age of COVID-19
The COVID-19 pandemic has inflicted a lot of collateral damage on society, particularly for health care services not related to the virus. University of Cincinnati researchers publishing in the Journal of the American College of Surgeons outlined the damage done to their lung cancer screening service and what they did to fix the problem.
According to the researchers, 800 scans were canceled during the three months the program was shut down in the spring of 2020. Even when the program reopened, monthly visits for low-dose computed tomography (LDCT) screening for lung cancer dropped markedly compared with pre-pandemic numbers. New patients were less likely to come for screening, and screening cancelations were significant.
However, the percentage of patients with lung nodules suspicious for malignancy went up from 8% pre-pandemic to 29% in June.
The program has since implemented a couple of changes aimed at making patients more comfortable with screening. First, they moved from an inpatient location to an outpatient setting. Second, they implemented new safety measures, such as enforcing social distancing in the waiting room and scanning areas and spacing appointments to clean those areas between patients. They enlisted program nurses and coordinators were to get the word out to patients about the increased safety precautions.
“We have to make sure as health care providers that we’re taking care of patients who have COVID-19 and along with the rest of the population who don’t have COVID-19, and that those two patient populations can safely co-exist and receive treatment,” said lead author Robert M. Van Haren, MD, MSPH, FACS.
Community Prevalence Matters
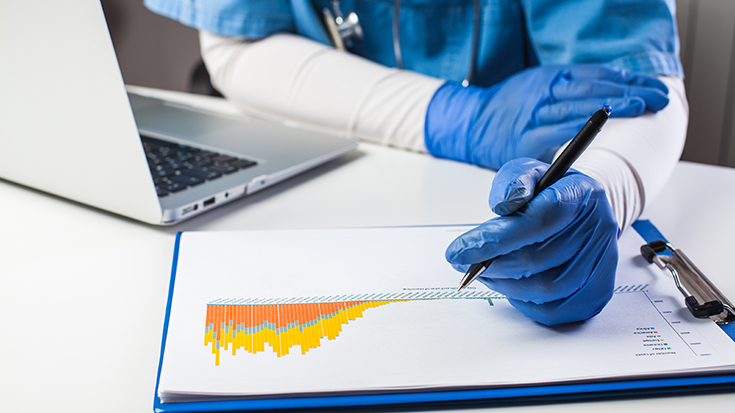
The death rate from COVID-19 has improved markedly since the beginning of the pandemic. New treatments like dexamethasone and better management of oxygenation have rightly taken a lot of the credit.
Researchers from the University of Pennsylvania and UnitedHealth Group believe the prevalence of COVID-19 in the community in question has played a significant role. When they compared mortality rates for COVID-19 at 398 hospitals across the nation during two time periods — January to the end of April and the beginning of May through the end of June — they found the mortality rate dropped from more than 16% to about 9%. Overall, 94% of the hospitals improved their mortality rate by 25% or more.
When they looked at the data based on COVID-19 prevalence in the counties where the hospitals were located, they found hospitals in counties where the prevalence declined over time showed the most improvement in disease mortality rates. “If it is the community burden of COVID-19 that determines how well our hospitalized patients do, as our study shows, then the best advice hasn’t changed: stay apart, wash your hands, mask up,” said lead investigator David Asch, MD, director of the Center for Health Care Innovation and a professor of medicine at the University of Pennsylvania. “Hospitals need our help.”
The study was published in JAMA Internal Medicine.
Email newsroom@aarc.org with questions or comments, we’d love to hear from you.