When the pandemic hit, it quickly became apparent to clinicians worldwide that being in the same room with a COVID-19 patient carried significant risk. Of course, no one knew for sure the size of that risk, but minimizing the number of people in the room became paramount as hospitals scrambled to come up with the best ways to ensure these patients received high-quality care while keeping essential workers as safe as possible.
At the University of Pennsylvania Health System (UPSH), health officials decided one way to accomplish that goal was to make greater use of telehealth services. They already had a tele-ICU program called PENN E-LERT in place, and it only made sense to add respiratory therapists to the mix.
Not a moment to waste
“Like many other institutions, we needed to think outside of the box,” said Steven Gudowski, BS, RRT, ASQ, CSSGB, director of patient safety at the Hospital of The University of Pennsylvania (HUP). “We already had a well-established working relationship with our telemedicine colleagues and decided to explore having an RT at PENN E-LERT.”
Karsten Roberts, MSc, RRT, RRT-ACCS, FAARC, education clinical specialist, and research coordinator at HUP, says the program set out to accomplish three main objectives. First, keep staff safe.
“We didn’t know how many staff would be infected,” he said. “Keeping them out of the rooms as much as possible was key.”
Second, they wanted to boost staff numbers.
“The less people in the room, the more we could focus on other areas and more acutely ill patients,” he said.
And third, they felt that the eRT service would help change RT practice for the future.
“This was a great opportunity to show value efficiency in respiratory care,” said Roberts.
Things moved at warp speed once they decided to launch the service.
“Within 24 hours, we mapped out our standard operating procedure and how we would staff the eRT the following week,” Gudowski said. ”It was my honor and pleasure to be a part of this amazing team that established an entirely new program overnight.”
Expanding the service
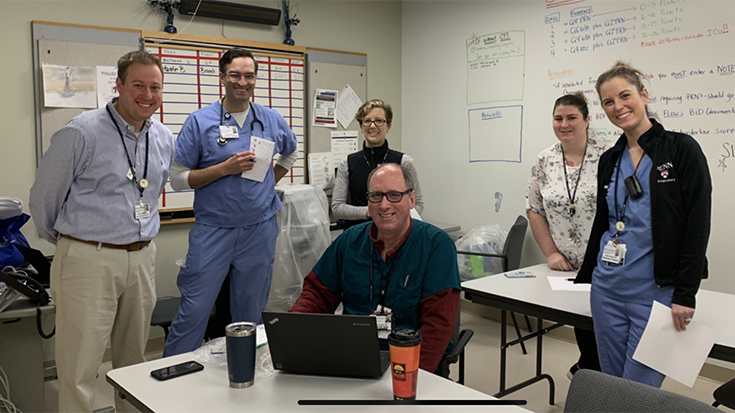
The eRT service was initially staffed by three RTs — Karen Zumstein, BSRC, RRT, RRT-ACCS, Anthony Jackominic, BA, RRT, and Amanda Shuttleworth, BS, RRT, RRT-ACCS. They were scheduled for eight-hour shifts while the team gathered baseline data on the effectiveness of the eRT role.
“We eventually expanded to eight RTs providing around-the-clock care,” Roberts said. “The eRTs now cover six hospitals in our health system, which includes 320+ ICU beds.”
eRT interventions read like a state-of-the-art ICU playlist. Therapists provide care according to an evidence-based bundle that includes ventilator liberation protocols, low tidal volume protocols, tube patency, and an extubation checklist. Proactive rounding takes place, complete with ventilator checks.
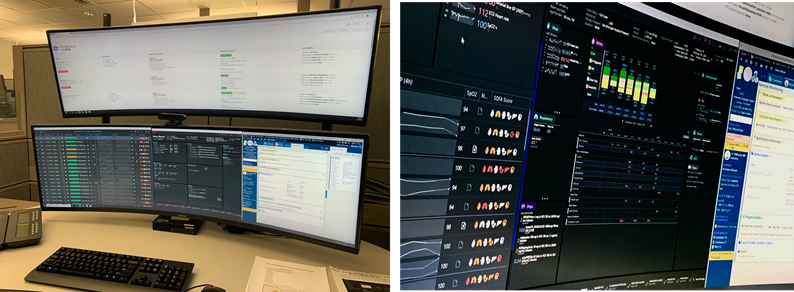
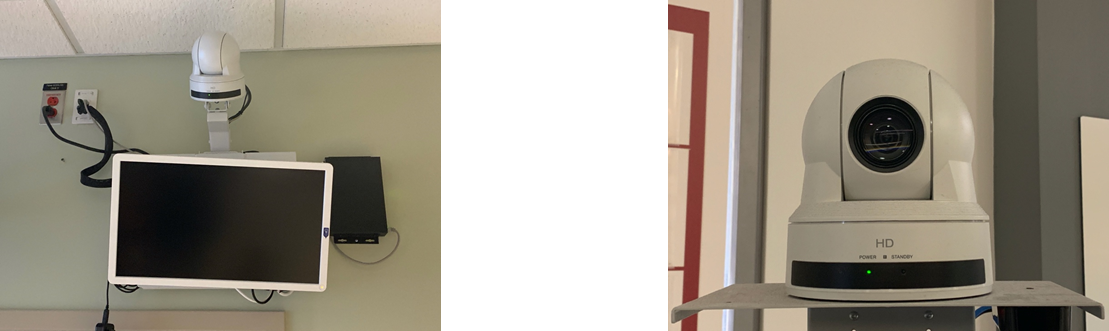
“The eRT is located two miles from the main hospital,” Roberts said. “The RTs interact with patients and clinicians in the ICU via a proprietary video monitoring system.” High definition cameras are in all ICU rooms, and therapists can zoom in on the ventilator to monitor waveforms, document settings, and identify any issues or concerns.
The value of the service has made itself evident in the individual patients who have received care via the program — and not just COVID-19 patients either.
Zumstein recalls one asthma patient who was intubated and receiving scheduled Q2 breathing treatments. However, the eRT noticed that the Aerogen was placed behind the HME, so the patient wasn’t receiving the medication.
“The eRT immediately alerted the bedside RT, who came to the bedside at once and repositioned the neb to where the med would reach the patient,” she said.
In another case, an eRT doing a routine ventilator assessment found that the patient was receiving double the maximum dose of Veletri. The bedside RT was called to the bedside to correct the value on the pump.
“eRTs have prevented multiple self-extubations by alerting bedside staff of patients who were moving or reaching for their ETTs,” added Zumstein.
Documenting the value
A study conducted by the RT team with colleagues in other disciplines was published in the Journal of Clinical Medicine in January 2022. It put some numbers to the use of the service.
Using a standardized data collection sheet to facilitate the review of medical records, direct audio-visual inspections, and direct interactions with the staff, they looked at 1,548 patients who received eRT services in May of 2020.
The results showed —
- 93.86% of the patients were coded as “routine” based on established workflows, 4.71% as “urgent, and 0.26% “emergent”; 1.17% were missing descriptors.
- The average intervention took 6.1 ± 3.79 minutes.
- In 16% of the interactions, no communication with the bedside team occurred.
- The eRT connected with the in-house RT in 66.6% of all the interventions, followed by house staff (9.8%), advanced practice providers (2.8%), and RNs (2.6%).
- Most of the interaction took place over the telephone (88%), secure text messages (16%), or the audio-video telemedicine ICU platform (1.7%).
- 5,115 minutes were spent on tasks that a bedside clinician would have otherwise executed, reducing their exposure to COVID-19.
A vital part of the team
The eRT is still going strong today and has even grown in scope. A service that was born out of the need to perform virtual ventilator assessments to save PPE and limit the exposure of bedside staff has evolved into one aimed at ensuring the highest level of care reaches all patients in the ICU.
“While they still help with routine ventilator assessments, eRTs are now vital team members that help support bedside staff and aim to improve quality and consistency of critical care delivery by adhering to best practice bundle compliance,” said Karen Zumstein. “The eRT is now responsible for completing the pulmonary bundle for all intubated ICU patients at UPHS.”
Tasks in the bundle include coordinating SAT and SBT trials and ensuring that every intubated patient’s extubation risk screen and plan are completed, and the appropriate visual cues are in place. The bundle also calls for all newly extubated surgical patients to have an order for the bronchopulmonary hygiene protocol and the documentation of an inspiratory capacity within six hours of extubation.
Lastly, eRTs ensure that the lung protective ventilation protocol has been ordered for confirmed ARDS patients and that these patients follow low stretch guidelines.
Tips to consider
Zumstein believes other hospitals and hospital systems could benefit from an eRT service similar to the one implemented by UPHS.
“While some of PENN E-LERT’s work is reacting to deteriorating physiological parameters and actioning timely intervention, the increasing work is helping bedside staff with best practice bundle compliance, which is more important than ever with the burnout and short staffing that has been plaguing frontline workers,” she said.
Karsten Roberts has three good bits of advice for any hospital that might be interested in putting an eRT service of their own into operation.
- Realize that there are limitations that cannot be avoided. Penn Medicine invested in the PENN E-LERT program more than a decade ago. So, we had the infrastructure in place to be successful.
- Create buy-in among the stakeholders. This requires a lot of education for the clinicians “on the ground.” They need to understand what the mechanism is and how it should be used. They also need to understand the role of the telemedicine clinicians — what they can and cannot do from afar and how they can be of assistance.
- The RTs involved should have 5-10 years of experience in critical care, along with advanced credentials. You want to have RTs with a high degree of critical thinking and communication skills.
An extra layer of support
A telemedicine service such as the one in place at UPHS may seem futuristic to many. Yet, as these therapists show, the future can be now for those who take the plunge and harness the power of technology to improve care.
Said Karen Zumstein, “We provide an extra layer of clinical support for our hardworking bedside staff to ensure that our patients receive excellent care.”
Email newsroom@aarc.org with questions or comments, we’d love to hear from you.