The landscape of the health care paradigm has been forever changed by the Coronavirus Disease 2019 (COVID-19) pandemic, challenging professionals across the globe. Along with other intensive care professionals, the respiratory care profession sits at the top of the provider platform when treating these patients. Respiratory therapists could be found on progressive care units, emergency rooms, or the intensive care units (ICU), specifically caring for the COVID-19 patient.
However, what if we need to transfer these patients to a higher level of care? For example, how could a community hospital care for a rapidly declining respiratory patient in prone-positioned and possibly needing extracorporeal membranous oxygenation (ECMO) intervention? Is it safe to transfer these patients? What precautions are taken? These are all questions faced by transport programs across the world, including Italy, Germany, France, and the United States.1
This specific article will strictly refer to inter-facility transport via ground (CCT), rotor-wing (RW), and fixed-wing (FW) modes of transport. The highlights will include how the air medical professionals, including the respiratory therapist, faced the challenges of transporting the sickest of the sick.
Challenges
In January 2020, the first COVID-19 patients began to appear in the northwestern and western parts of the United States. While these were defined as isolated cases, the pattern of this rapidly transmissible virus throughout the country became evident. Further, the insult it inflicted on the respiratory system and the requirement of ICU level care for these patients was sure to stretch ICUs and hospitals to their breaking points.2 With this being the case, patients required transfers to higher acuity tertiary care centers where these patients could receive higher level of care. The imposing questions for transport providers and hospital-based transport programs became glaring: How can this be done safely? Should it be done? What lessons have been learned so far? How do the transport providers remain safe? From an RW and FW perspective, there was a perceived industry-wide “time-out” to gather as much information and clinical data as possible on if it was safe to transport these patients. All we knew was this was a highly transmissible and infectious virus that attacks the respiratory system. There was a lack of data to guide the Helicopter Emergency Medical Services (HEMS) industry, air medical professionals and those emergency medical professionals in the pre-hospital setting. Critical Care physicians, emergency physicians, air medical directors and crew, and industry vendors held weekly virtual meetings to discuss and share current knowledge and practices amongst fellow programs. As the team collaboration was evident in the ICU, it was eminently clear this would be the case in the air medical transport realm, that this was going to be a TEAM effort. The medical crews need to protect themselves, the pilots, the mechanics, the oncoming crews, and the aircraft, ambulance, or helicopters interior required high level disinfection. Standard Operating Procedures (SOPs) had to be newly written, while others needed to be updated or changed. Patient care protocols required development or revision to accommodate the transport of these patients. The effect this had on some programs was nearly a 75% drop in transport volume in the early phase of this pandemic, simply because the unknown was one of the most significant challenges.3
To further complicate the safe and successful transport of these patients, many were benefiting from prone-positioning and advanced mechanical ventilation settings. So, subjugating these patients to the abandonment of their current standard of care, with the result being a transfer to a higher standard of care, was equivalent to disaster! Transport teams needed to include the appropriate staff, equipment, space (“space, staff, stuff”), and absolute team “buy-in.” The transport team and service must provide, at the minimum, the same level of care the patient is receiving at the referring facility. This ensures the crew can deal with an acutely critically ill, highly infectious patient in a confined space. The crew must be competent in medication and airway management, advanced ventilation modalities, and be prepared for airway emergencies that may potentially arise. A Transport Team member highly qualified in advanced mechanical ventilation settings and knowledge of the ventilator platform being used and concomitant therapies (i.e., inhaled pulmonary vasodilators, PEEP strategies, proning, etc.) needed to be involved. While remaining an underused resource in the inter-facility transport of the difficult respiratory patients, the respiratory therapist remains an essential resource and member of some transport teams.
Questions
There remained significant questions about transporting the COVID-19 patient, whether there was a known positive result or just a person under investigation (PUI). The first question was, what would be the proper personal protective equipment (PPE)? RW transport personnel wear helmets in flight, so some hood coverings could interfere with communications. We established early on that the PPE would consist of hair covering (surgical cap, skull cap, or similar), goggles, N-95 or equivalent face mask, protective suits or gown, and boot coverings.4 While this seems like a simple donning procedure for CCT and FW crews, the RW arena would once again present communication issues while attempting to communicate with a voice-activated microphone through the N-95 mask or similar respirator masks. One of the critical components of transporting the COVID-19 patient is communication amongst crew and pilot(s).3

Air medical crew with PPE.
The second question was if the patient was able to be transported safely. While a significant number of patients were not intubated, it was the sickest patient population that required ICU-level care while in a very confined space with limited resources. In other words, should the mechanically ventilated, prone-positioned patient on inhaled pulmonary vasodilators, with +18 cm H2O of PEEP, and four, or six, or eight different intravenously infused medications be placed in an aircraft or ambulance for a potentially extended period of time? Should the patient be placed in the supine position? What if the supine position failed? Communication not only in transport was important, but before the transport even began was just as important. The crew retrieving the patient must be well versed in ICU-level care and be well informed of the patient’s most current condition. It is also noted that patients don’t stay in the prone position for 24 or 36 consecutive hours, or at least they shouldn’t. There is a period of placing the patient in the supine position. It would be prudent for some patients to defer the transport until the patient was placed supine and stable before taking the patient out of that environment. Not all CCT or transport services can offer these patients the critical care level required, hence why the ICU RN/RRT crew makes sense. If there is ever a doubt in crew capability or mode of transport to be used, then strong consideration to defer or even decline the transport should be given.
Lastly, the third question relates to the possible exposure risk to crew and patient isolation. While commonly used in FW and some CCT arenas, the isopod device was not tenable for most RW programs. Therefore, some programs absolutely refused to transport COVID-19 patients with respect to crew exposure. While mechanically ventilated patients with a closed system and appropriate high efficiency particulate air (HEPA) filtration are the safest, they were not the majority of patients transported in the RW environment. The continued concern for crew safety was always of paramount consideration when deciding how to transport these patients safely. Patients who were not on a closed ventilatory system (i.e., nasal cannula, non-rebreather, heated high flow nasal cannula) were also masked with an N-95 or appropriate procedure mask for transport. In addition, there was a strong concern regarding exposure to the crew via aerosol-generating procedures, such as non-invasive positive pressure ventilation (NIPPV), continuous positive airway pressure (CPAP), or heated high flow nasal cannula (HHFNC). Because of these initial concerns, these procedures were strongly discouraged and, these deferments may have directly contributed to ventilator shortages in some “hot spot” areas of the country (Darren Braude, 2021). There remains an extremely low exposure to infection ratio for air medical crew, and standard PPE remains effective, even with the use of NIPPV and HHFNC.4
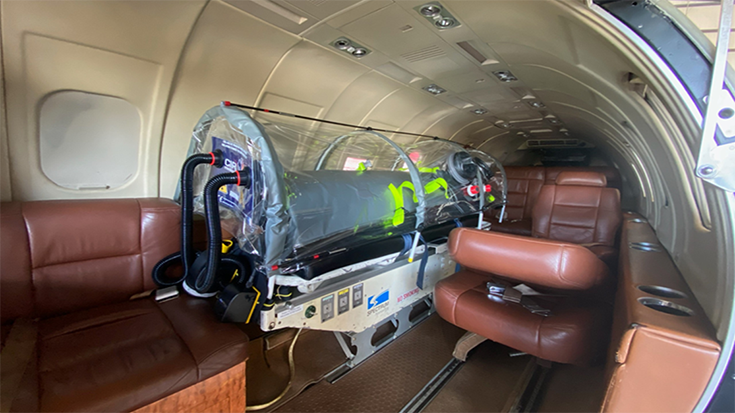
Isopod device in the fixed-wing environment. Photo courtesy Jet I.C.U.
The cleansing and safe return of ventilator equipment was also addressed. It should be noted that many ventilator platforms are used in air medical transport and these devices should be cleansed per manufacturer guidelines. As a reference, this program utilizes the Hamilton T-1platform (Hamilton Medical, Reno, Nevada). After each use, the ventilator surface is thoroughly cleansed with appropriate disinfectant wipes. The reusable exhalation valve is also disinfected per manufacturers recommendations.
Conclusion
The safe and effective transport of the COVID-19 patient and PUI’s can be performed successfully. While early in the pandemic there needed to be questions answered, the air medical and critical care ground transports of these patients have been effective, with extremely low infection to exposure ratio for transport crew. While the transport of treatment adjuncts such as prone positioned patients’ needs to be subjectively considered, it remains a high-risk transport risk. Therefore, it is not routinely performed in the air medical theater. Some programs perform these transports with a critical care ground crew. However, we need to consider many aspects of patient care before these transports are accepted and take place (e.g., ventilator settings, airway and sedation control, infused medications, and patients’ risk of hemodynamic compromise prompting a rapid supine position). Patients that are prone positioned in need of higher-level care should be deferred until a supine position can be safely achieved, at least for the time the patient will spend out of the hospital.
The intubated and mechanically ventilated patient is not the most frequently transported patient; however, when the critical nature of these patients requires ICU level care, there needs to be an ICU level team. This is one of the major factors considered when transport programs are asked to transport these high acuity patients. Can this team offer ICU-level care? Do we have the appropriate equipment and transport method afforded to the patient? And can it be delivered, along with the patient, safely to the receiving hospital? All crew members need to be well versed in advanced ventilation approaches, inhaled pulmonary vasodilators, vasoactive infused medications, possible patient decompensation and/or airway emergencies, and plans in place to address these issues without major exposure risks (i.e., transferring from ICU ventilator to transport ventilator, PEEP considerations and clamping of endotracheal tubes). Delivering the patient in stable condition, or even a better clinical condition than before transport is the absolute goal of all transports.
There have been many lessons learned since this pandemic started, and we will continue to learn new lessons. The transport of these patients is a common practice, and many programs are now providing these transports. Yet, some defer these transports to other programs or use a ground transportation team to complete the transport. Providing considerations are made with reference to the patient’s condition and out of hospital time, the mode of transport is not a major contributing decision factor. It’s the team put in place to complete the mission safely and successfully. That’s all the patient asks!
References
- Stefan Sammiti, J.T. (2021). Analysis of European Air Medical Evacuation Flights of Coronavirus Disease 2019 Patients. Air Medical Journal, 211-215.
- https://covid.cdc.gov/covid-data-tracker/#datatracker-home. (2021, July 15). Retrieved from https://cdc.gov/coronavirus/2019-ncov/index.html: https://cdc.gov/coronavirus/2019-ncov/index.html
- Martin, D. T. (2020). Fixed Wing Patient Air Transport during the Covid-19 Pandemic. Air medical Journal, 149-153.
- Darren Braude, M. L. (2021). Safety of air medical transport of patients with COVID-19 by personnel using routine personnel protective equipment. Journal of the American College of Emergency Physicians, 1-5.
- Claude Guerin, J.R. (2013). Prone Positioning in Severe Acute Respiratory Distress Syndrome. New England Journal of Medicine, 2159-2168.
Email newsroom@aarc.org with questions or comments, we’d love to hear from you.