
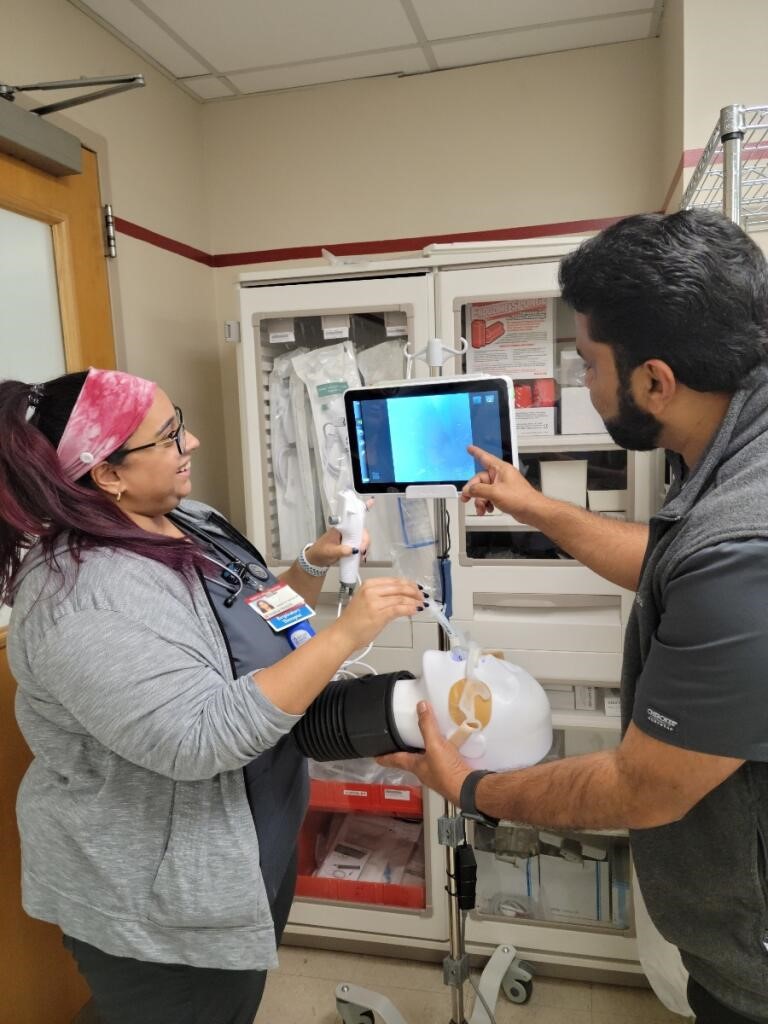
Senior RTs Colleen Swearingen, left, and Reshma Nair, right, watch as Anoop George reviews aspects of the bronchoscopy selection process.
Earlier in 2021, bronchoscopies at Temple Health in Philadelphia, PA, were performed in the bronchoscopy suite by physicians who selected the scopes solely at their discretion. The result? A big expenditure for the cost of disposables.
The multi-hospital system then embarked on a mission to become one hospital with many campuses. In doing so, efforts to standardize processes and streamline care wherever possible put that practice under the microscope. This examination discovered room for improvement, and respiratory therapists were called into action to help make it happen.
In the end, the hospital had implemented a bedside bronchoscopy program using RTs as gatekeepers to select the scope, resulting in a safer practice with significant savings in expenses.
Integrating the teams
“Temple University Hospital implemented the bedside bronchoscopy program to incorporate the pulmonary provider team and the bedside respiratory team,” explained Anoop George, RRT, assistant manager for respiratory care at the main hospital campus. As a result, critically ill patients who meet the criteria for a bedside bronchoscopy can receive the procedure in a more timely fashion, minimizing any delay in the provision of care.
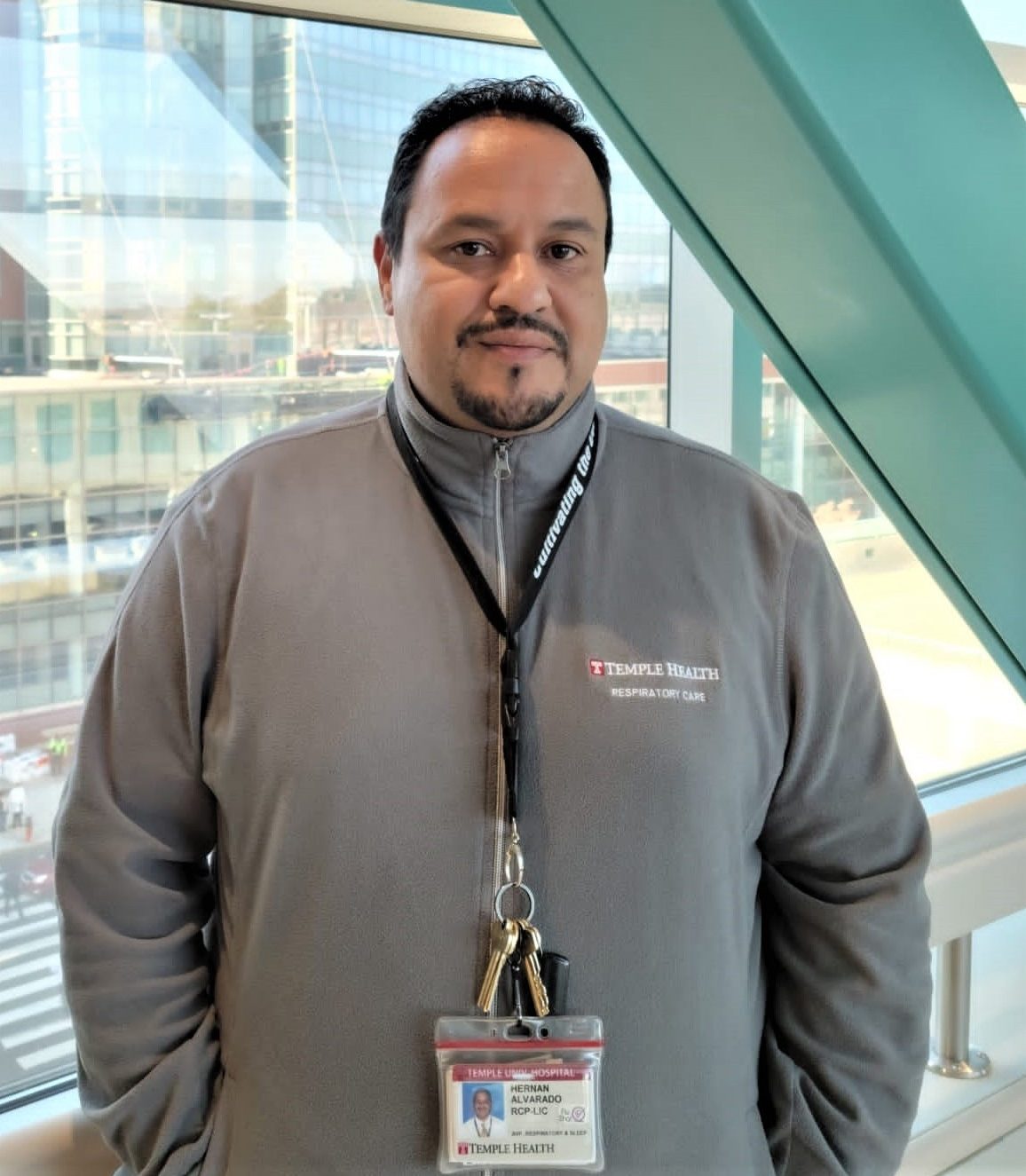 Hernan Alvarado believes the disposable bronch project has created a greater partnership between the inpatient and outpatient RTs at Temple.
Hernan Alvarado believes the disposable bronch project has created a greater partnership between the inpatient and outpatient RTs at Temple.Hernan Alvarado, Jr., MBA, RRT, RPFT, associate vice president of respiratory care and sleep diagnostics services, notes the bronch service line is not a part of the RT department. However, diagnostic RTs do play an integral role in the bronchoscopy suite. Therefore, the process change required the involvement of several departments within the hospital, including project management, respiratory care, and central supply.
Pulmonary, trauma, and burn physicians were also essential to the process.
“The respiratory therapists became the gatekeepers for bronchoscopy in general,” said Alvarado. “We developed criteria that ensured the correct reusable or disposable scope was available for the provider.”
Those criteria include airway size, patient acuity, the feasibility of transport, and COVID-19 status.
Excellent outcomes
The process begins with discussing the patient’s needs during rounds and the pulmonary team deciding if the patient is suitable for a bedside bronchoscopy. The respiratory team takes it from there, acquiring either disposable or reusable devices based on the pre-determined criteria.
 Clinical Supervisor Roy Thomas, right, points out an interesting finding on the screen to Senior RT Reshma Nair.
Clinical Supervisor Roy Thomas, right, points out an interesting finding on the screen to Senior RT Reshma Nair.“All COVID patients and those on droplet precaution will have a disposable scope available,” said Anoop George, noting only essential practitioners will be at the bedside for these procedures to minimize exposure risk to staff. “Non-isolation patients will use the reusable bronchoscopes.”
After the team implemented the new process, Temple saw a 33% reduction in disposable usage and improved collaboration between the RT and provider teams. Additional results included optimized care and a 50% drop in emergency procedures.
Anoop George says the teaching opportunities that have arisen due to the process change have been invaluable too.
“Six months into the initiative, and after several education sessions focusing on the RT department, we are better at recognizing the changes in patient status, and reviewing X-rays have resulted in early identification for these procedures,” he said.
No project without RTs
Sean Duffy, MD, associate professor of clinical thoracic medicine and surgery at the Lewis Katz School of Medicine at Temple and a practicing pulmonologist, says RTs held the key to the success of this project. “RTs were the backbone,” he said. “They became the method of implementation of the whole project as the providers and keepers of the scopes.”
 Tanya Cofield, left, Clinical Performance Manager Lou Fetscher, Sr., center, and Performance Excellence Manager Britany Layton, right, were all involved in making the disposable bronch project a success.
Tanya Cofield, left, Clinical Performance Manager Lou Fetscher, Sr., center, and Performance Excellence Manager Britany Layton, right, were all involved in making the disposable bronch project a success.Indeed, had therapists not been available to properly set up the equipment in a timely manner, he believes the project would have never come to fruition.
According to Dr. Duffy, therapists increased scrutiny regarding which scope to use for which patient. In addition, communication between team members improved in day-to-day patient care and respiratory needs thanks to the RTs’ greater familiarity with the patient.
“The fellows and attendings may have been seeing the patient for a day prior to a procedure, but the RT may have been with the patient for a week or more in some cases,” he said. With the two teams in improved communication, it was only natural that clinical information would make its way to the physicians sooner than it otherwise might.
Tips for successful implementation
Dr. Duffy says he would absolutely recommend a similar initiative to other hospitals. “It has improved communication, uniformity, patient care, and of course cost-efficiency,” he said. “Also, it was a very smooth transition that I believe was mutually beneficial for respiratory therapy and the pulmonary providers.”
Tanya Cofield is the bronchoscopy supervisor at Temple. She wholeheartedly agrees, noting that bringing bedside RTs together with those on the diagnostic team greatly impacted patient care. It also greatly facilitated team building within RT ranks in the hospital.
“We are all therapists, and we can and should function as one,” she said. “Whether you are in a procedural area or an ICU, we all have similar backgrounds and training. We just use different aspects of our training depending on our work assignment.”
Hernan Alvarado says that the melding of RTs in the inpatient and outpatient diagnostic areas was one of his objectives in pursuing the project from the outset, and he is happy to see how it turned out.
“It was my goal to bring the inpatient RTs and outpatient diagnostic RTs together as partners on the same team,” he said.
He shares these four tips for the successful implementation of a project, such as the one developed to rein in costs for disposable bronchoscopes at his hospital –
- Engage all staff and other stakeholders in the process.
- Educate staff about their role as vital members of the clinical team.
- Empower staff to steer the correct care and safe delivery of services to patients.
- Follow up. Look at what has been working and what needs to be adjusted, and keep open lines of communication across the entire team.
Collaborative effort
The disposable bronch project implemented at Temple Health is an excellent example of how RTs can use their expertise to work collaboratively with physician providers to affect cost savings. By acting as the gatekeepers to the supplies used in the process, they save money for their hospital while improving the timeliness of bronchoscopies at the same time.
Email newsroom@aarc.org with questions or comments, we’d love to hear from you.











