Jim Damron, MDiv, MBE, RRT, CPFT, seriously considered medical school during his undergraduate years, but his love of the water got in the way. The summer after he graduated from college was spent in the Florida Keys, swimming, sunning, and training as a Scuba diving instructor.
“Yes, tough life,” he says now with a smile.
After a few years of teaching and managing dive shops on the beaches of Florida and North Carolina, though, he found his passion for medicine remained. A couple of his dive students worked in the medical field, and they encouraged him to take a closer look at the pulmonary field due to its similarities to diving.
“Fast-forward 25 years, and I had worked in several different aspects of the respiratory discipline, including critical care, long-term care, and pulmonary function,” Damron said. Then he got an opportunity to invest more of his time and energy into teaching. Equipped with his RT education and master’s degrees in theology and bioethics, he decided it was time to combine both of his passions in life into one to help improve the care of caregivers like RTs.
While he still works part-time as an RT to maintain his clinical skills, he spends much of his time speaking and coaching professionally, including on the topics of burnout and medical ethics. We asked him to share his insights into what it takes to keep going even when a pandemic like COVID-19 has turned your world on its end.
How has the pandemic impacted RTs?
Three things come to mind: Exposed, Highlighted, Reminded.
Exposed: COVID-19 exposed to the public the high demands that face RTs daily. Like many health care providers, RTs are often short-staffed, undervalued, and care for patients in critical and terminal situations. These constant demands usually keep RTs on the edge of burnout. The pandemic exposed that RTs are often on the verge of collapse on any given day. COVID-19 happened to be the additional strain on this shaky house of cards, causing it to tumble.
Highlighted: The pandemic also highlighted the importance of having pulmonary specialists. I think RTs have been undervalued for too long, and the pandemic, though horrible, highlighted just how vital respiratory therapists are. The question now is, how best to use this awareness to further the discipline?
Reminded: The virus also reminded us that we are vulnerable. In addition to the constant stress involved in working as a frontline clinician, RTs must never take their vocation for granted. Dealing with sickness, disease, and death takes its toll whether you realize it or not. You can’t care for others if you don’t care for yourself. As a dive instructor and former marine taught me years ago, a good hero is not a dead hero.
What do RTs need in terms of support?
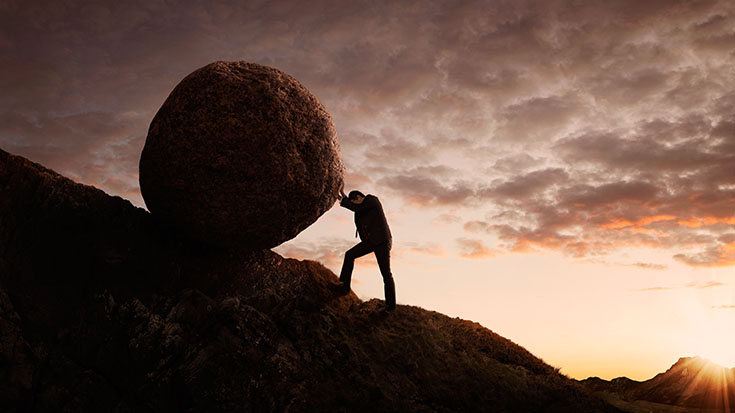
Burnout occurs when demands exceed resources, but it is not the problem. Burnout is a symptom. The best support we can provide our staff and each other is to communicate how valuable RTs are and invest in them as experts in their field.
Value: Communicating value is one of the best ways to increase resources when demands are high. One can communicate value by 1) privately thanking someone, 2) publicly acknowledging them, and 3) providing them an opportunity to excel. One of the reasons I have remained in the respiratory field is because I have had managers and directors who have allowed me to showcase my passion and interest in teaching.
Investment: Investing is another way to show support. Investment can take the form of listening to RTs’ concerns, providing opportunities to grow their skills and competence, and even financial incentives. But a word of caution about money. Money is a great motivator, and no one will refuse increased compensation. But money rarely fixes the problem. Instead, it can sometimes be viewed as a bribe to convince others to tolerate increased demands.
These two mechanisms of support can yield fast results. But to reduce caregiver burnout, we have to decrease demands on the RT. Reducing is an individual and organizational responsibility. Individually, RTs need to understand what drains them and what refuels them.
Organizationally, the support is more challenging. But can you imagine if an organization declared they were taking the national average of RT/patient ratio (or RN/patient) and cutting it in half? That would send a clear message of value. During the pandemic, this becomes increasingly important. It isn’t easy to walk away from a position and a vocation where one feels fully valued and appreciated.
What are 3-4 coping strategies RTs can use to push through?
Person: I like to categorize stress into two groups: lifestyle and life situation. By and large, you cannot control life situations. Tragedies, people’s opinions, pandemics, etc., are usually beyond our control. What you can control are lifestyle stresses. When I went through counseling and coaching training, we had a saying: focus on the person in the room. There is no benefit in worrying about things outside of your control. You can only control the person in the room — You. Focus on your lifestyle habits — nutrition, health, and well-being, and let go of the rest. It’s very liberating.
Punchline: A millennium of research shows that laughter is often the best medicine. Laughter reduces cortisol and increases dopamine levels, which counteracts the harmful effect of stress on your body. I like to listen to a favorite comedian or watch a show I know will make me laugh. And if you do this before you go to sleep, you will sleep better. Better sleep leads to better-balanced hormones, mood, and immune systems.
Empathy: Empathy imagines what it is like from another’s perspective. Sympathy conveys emotions and imagines someone’s perspective being their own. Empathetic RTs provide better quality care. But the increased virtual world resulting from technology and the pandemic has reduced our empathy capacity to negligible levels. Grow this skill by asking yourself, what is life like for your patient? Your boss? Your employee? Practicing this awareness daily on your drive home or periodically in written form can maintain your ability to show compassion and protect you from burnout (Note: if you choose to write down your thoughts, you could end up with a collection of publishable stories!)
Final Words
According to Jim Damron, the pandemic has revealed much about our society and the people who live in it. It has also illustrated our capacity to handle adversity.
“Remember that if you are experiencing some degree of burnout, it may take time to recover,” he advises his fellow RTs. “Burnout is usually a gradual process, so understand that it will be a gradual recovery. Never forget that you make a difference. Don’t let burnout prevent you from impacting others the only way you, the RT, can.”
Learn more about Jim Damron on his website, JimDamron.com.
Email newsroom@aarc.org with questions or comments, we’d love to hear from you.