It isn’t every day that I see a product offered that enhances a provider’s patient care and serves a risk management function. As I have said before, risk management is everyone’s job, and unfortunately, when everyone has the responsibility, often no one has the responsibility. You see this every day in health care operations where patients ask a housekeeper to send in the nurse, and the housekeeper says, “not my job: use your call bell.” A common theme in all my risk management presentations has been that it isn’t the act of negligence that gets most health care providers sued; it’s the way the patient feels about how he was treated.
Some patients do not want and do not need hand-holding. I’m one of those. I have an insulin pump and an advanced degree. My fingers know how to push buttons, and I can read numbers off a glucose monitor. When a nurse or other health care provider tries to “help” me with these difficult tasks, I often snarkily inform them (and I’m not proud of this) that English is my native language and that I wasn’t dropped on my head at birth. I am quite possibly the worst patient in the world because I have a health care background.
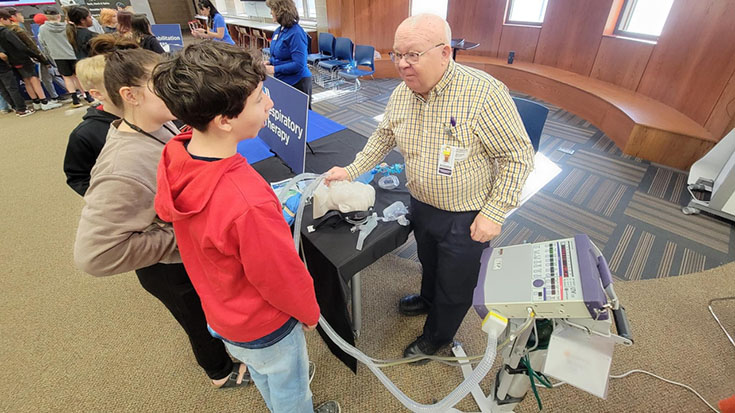
Most people have no such health care background and are a bit less irritable. Their health care providers, particularly respiratory therapists, tend to be people with whom they develop a close relationship. It’s one reason many respiratory care programs emphasize communication skills and active listening. Being able to have a quality conversation that produces actionable information is vital to meeting patient needs. Very few products or services fill this role.
Recently, however, I came across a service by HGE Health. HGE Health is a Vapotherm company that has taken a different path from most service companies working in the healthcare field. Most companies tend to focus on serving as many markets as possible, offering a set number of services per discipline, and adapting their baseline service to different markets. An example illustrates the problem with this approach.
Back in 1961 (a time before Broadband, if you can believe that), a company called Amphicar introduced a car that was also a boat. It would run on land and water, so long as the water was relatively flat and peaceful. You can still find photos of it on the internet. But the problem was, it wasn’t a good car, and it wasn’t a good boat. It was a car-boat. That is, unfortunately, the state of the art for many people merging software and patient care services in health care.
HGE Health has taken a different approach with two products aimed specifically at physicians and programs providing health care to COPD and COVID-19 patients. Instead of doing many things at a C+ level, HGE has taken the path of doing one thing at the A+ level. It provides a system that remotely monitors COPD patients based on clinically-validated science and uses changes in condition to engage in active intervention to improve clinical picture and quality of life. It adapts the science of Dr. Gerald J. Criner of the Temple Lung Center and has been very successful. A COPD patient evaluates their temperature, peak flow, sputum production, and breathlessness and inputs that data on a smartphone app that sends the data to a central collection hub. Based on the patient’s history and their current status, the system flags certain changes for clinicians’ calls. The clinicians use common clinical interventions consisting of antibiotics and, if necessary, steroids to prevent the disease progression before hospitalization is required.
Clinically, the program can be a lifesaver. But from a risk-management point of view, it can be a great litigation avoidance tool. The one thing that patients all say when they see a malpractice attorney is this: “the doctor [or therapist] wouldn’t listen to me.” I have seen this time after time and written about it frequently. With this tool, managed by allied health professionals, a physician or Pulmonary Rehabilitation program can honestly claim to always be listening to the patient. The system has worked so well for COPD patients that HGE has put together a separate tool for COVID-19 monitoring and early interdiction. The key is that each of these programs focuses on the pulmonary patient.
When I asked Mike Markus of HGE why he didn’t take this approach and adapt it to other diseases, his answer was simple and to the point: “we’re focused on the pulmonary patient. We want to do this one thing very well, not lots of things half-way.” As this tends to go against the Wall Street approach to make as much money as possible upfront and then sell out, it intrigued me. Here was a company whose desire was to produce real-world solutions for real patients.
Often COPD patients live alone. They may have family hundreds of miles and several hours away. Frequently when they feel themselves starting to have difficulty breathing, they have missed the tell-tale signs at the outset of the episode. They don’t call the doctor’s office until they are already short of breath. And, as I have seen with my own physicians, sometimes that provider doesn’t call back for 24 hours because calls get handled in the order they’re received and are not always triaged appropriately. However, by then, the patient is in the Emergency Department, and angry family members from Buffalo are wondering why the provider in St. Louis waited so long to do something.
Guilt is a powerful motivating force. As a lawyer, I’ve seen many family members say, “I can’t help what happened to my dad, but maybe I can prevent it from happening to someone else.” They sue not because there is some magical way to bring back their deceased loved one, but because they feel angry at the provider and, in truth, angry at themselves.
Now let’s roll that video back to the point where, three days before he called the doctor, he noticed increased sputum and entered that into the HGE app. The call center calls him, and over the next several days, monitors him closely, starting antibiotics on the second day, and steroids on the third day. The children in Buffalo never find out that Dad had a problem in the first place. The patient raves about the great team of clinicians taking care of him. And Zig Ziglar, the famous sales author and motivational speaker said that a patient is apt to tell up to 150 people over the course of a year about a good experience with a provider.
HGE Health probably didn’t set out to create a risk management tool. But that’s what they did.
Email newsroom@aarc.org with questions or comments, we’d love to hear from you.