We define Persistent Pulmonary Hypertension of the newborn (PPHN) as the failure of normal circulatory transition that occurs after birth. With PPHN characterized by severe pulmonary hypertension, blood vessels to lungs constrict, impairing gas exchange and right ventricular function. In children three months and older, pulmonary hypertension is defined as mPAP >25 mmHg.1 In this article, I review treatment strategies’ and discuss the benefit of combined pulmonary hypertension therapies.
Inhaled Nitric Oxide
Nitric oxide is a potent selective, pulmonary vasodilator. Its mechanism of action involves guanylyl cyclase activation, leading to cyclic guanosine monophosphate production, which results in smooth muscle relaxation. Wessel et al. did one of the first known clinical studies of children treated with postoperative PH. The study showed a three-fold increase in the plasma levels of cyclic guanosine monophosphate during the INO delivery. Nitric Oxide is often the first-line treatment for PH. In 1999, the FDA cleared nitric oxide of use for neonatal patients (> 34 weeks gestational age) with hypoxic respiratory failure associated with clinical or echocardiographic evidence of PH. Oxygenation index (OI=mean airway pressure MAP × FiO2 × 100÷PaO2) is used to assess the severity of hypoxic respiratory failure (HRF) and PPHN. Nitric is initiated in cases where OI is 15-25, suggesting moderate hypoxic respiratory failure.3 Off-label use of nitric oxide has improved oxygenation for critically ill patients of all ages, including adults. The American Academy of Pediatrics recommends administering Nitric Oxide under specific guidelines. Nitric should be prescribed under the direction of physicians qualified by education and experience in its use. It should also be used at centers with ECMO access or can transfer to an ECMO center rapidly.
A number other inhaled vasodilators have be used in addition to Nitric, I encourage you to consider your institution practice, as we explore the synergist benefits of combination therapy. This concept we apply daily in our novel treatment of bronchospasm with Albuterol and Atrovent.
Epoprostenol
Epoprostenol, a prostacyclin derivative, can help in the treatment of PH. Prostacyclin is a substance produced by vascular endothelium that stimulates adenyl cyclase in vascular smooth muscle cells resulting in vasodilation. Epoprostenol is FDA approved for IV administration only. Off-label use of inhaled Epoprostenol produces selective pulmonary vasodilation without affecting the systemic BP. Aerosolized PG2 has been shown to be effective in improving oxygenation and lower pulmonary vascular resistance in children with acute hypoxic respiratory failure and congenital heart disease.7 Several studies suggest that epoprostenol is just as effective as Nitric oxide. At my institution, a group conducted a study looking at its utility over 14 months. This retrospective study suggests inhaled epoprostenol as novel treatment in managing acute pediatric PH in critically ill children.8 In addition 75% of the patients studied had other adjunct therapies.8 Weaning protocols are recommended to reduce the incidence of rebound PH incidence. Some institution transition patients using Bosentan, ERA, as a bridge to weaning.
Bosentan is an endothelin-1 receptor agonist to inhibit constriction in the pulmonary vasculature, resulting in vasodilation. While used for adults for a while, Bosentan recently was proven effective treatment for pediatric IPAH, Idiopathic Pulmonary Arterial Hypertension. It was FDA approved for pediatric three-year-olds and older in 2017, based on the Breath-3 trial findings. The study reported pulmonary vascular resistance was drastically reduced in children age 3-15 years old treated with Bosentan.4
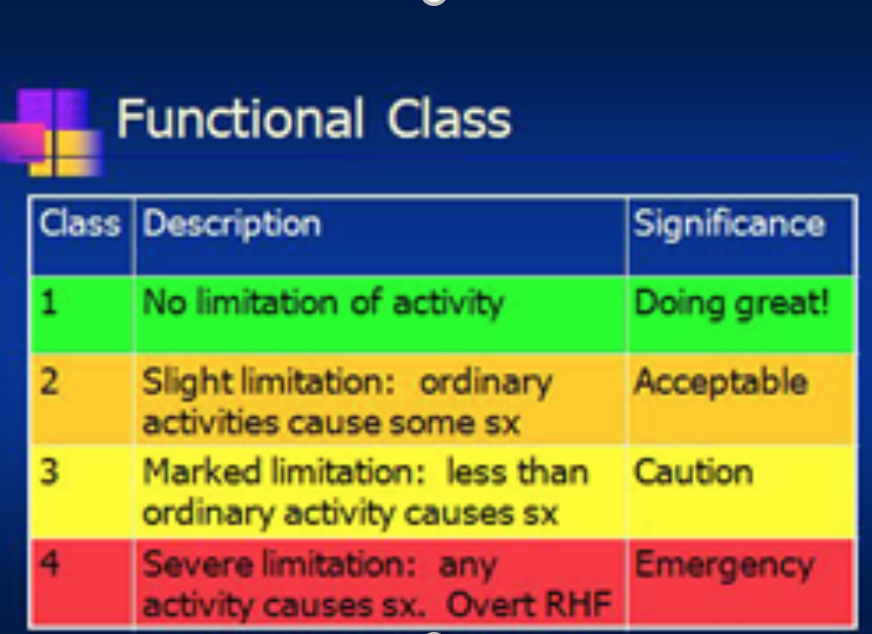
Treprostinil is a synthetic analog of prostacyclin that produces dilation of blood vessels. This drug targets the prostacyclin pathway. Treprostinil is FDA approved for IV administration. This therapy is sometimes used in transition from epoprostenol. Ush Krishnan et al. conducted RCT, which looked at the safety of inhaled Treprostinil in children.6 Patients received three to nine breaths of (6ug/breath) four times a day for six weeks. This small cohort showed improvement in exercise capacity and World Health Organization functional class (WHO-fc) Fig 1, when added to other targeted therapy for PAH. The WHO FC is a means of classifying PAH diseased severity. In addition, its often used, to guide patients’ management. Further studies suggest that Treprostinil is suitable for pediatric PAH.6 Also, Treprostinil inhibits inflammatory cytokines, which contribute to other forms of respiratory failure, i.e., PARDS, pediatric adult respiratory distress syndrome.
Sildenafil, PGE5 inhibitor, that works on the nitric oxide pathway. Phosphodiesterase type 5 is a molecule in the body that interrupts the production of nitric oxide. Sildenafil inhibits its ability to do so. Recent case report, oral sildenafil led to a dramatic improvement in exercise tolerance in adults. Off-label use in children is controversial. Early studies suggested favorable outcomes in children treated with sildenafil. It initially improved oxygenation and hemodynamic parameters.2 Sildenafil also help when weaning Nitric Oxide, minimizing the risk of rebound PH. Later studies, STARTS1 and STARTS2, suggest that high doses of in children may link to increased mortality.2
Role of Respiratory Care Practitioner
RCPs help physician colleagues in the care and management of these patients. Therapist are tasked with the duty of selecting adequate ventilation strategies, with minimal risk of lung injury. For example, HFOV, High Frequency Oscillation Ventilation, delivers small tidal volumes and high frequencies. The inhaled medications mentioned earlier are effective when delivered to well-ventilated lung fields. Continued assessment of patient vitals, such as Saturation, CVP, ABGs X-rays, Oxygen Index (OI), and End tidal CO2 help to direct management. Arterial blood gas gives the therapist information about oxygenation and ventilation. It also shows methemoglobin, which serves as an of the adverse effects of nitric. Nitric dosing can be managed and titrated. OI is used to assess the intensity of ventilator support needed to maintain oxygenation.2 (OI=mean airway pressure MAP × FiO2 × 100÷PaO2) Its often you used to determine the need for nitric oxide, as well ECMO. CVP (central venous pressure) monitoring tool that’s helpful in titrating nitric oxide and other vasodilators. Noninvasive monitoring tools are equally important. Rapid changes ETCO2 can indicate ventilation changes, that may be critical in manage PH. Abrupt changes in saturation can also be a clinicians first sign of PH crisis. Radiological studies lung expansion as well dilated pulmonary arteries.
Summary
In the past, clinicians rely on the evidence from adult studies to define pediatric patient care strategies. The AMBITION trial proved that combination therapy might provide clinical benefits in patients who do not benefit from a single class agent by targeting multiple mechanisms within the prostacyclin, nitric oxide, or endothelin disease pathway overall therapeutic effect.9 In the past decade, several RCT for the pediatric population have made treatment more precise.
References
- Kula S, Pektaş A. A review of pediatric pulmonary hypertension with new guidelines. Turk J Med Sci. 2017 Apr 18;47(2):375-380. doi: 10.3906/sag-1605-172. PMID: 28425226.
- Dunbar,Ivy. Pulmonary Hypertension in Children. Cardiol Clin. 2016 Aug: 34(3): 451-472
- DiBlasi RM, Myers TR, Hess DR. Evidence-based clinical practice guidelines: inhaled nitric oxide for neonates with acute hypoxic respiratory failure. Respir Care 2010: 55(12): 1717-1745
- Wang Y, Chen S, Du J: Bosentan for Treatment of Pediatric Idiopathic Pulmonary Arterial Hypertension: State-of-the-Art: Frontier in Pediatrics 2019: 7: 302
- Originally published3 Nov 2015https://doi.org/10.1161/CIR.0000000000000329Circulation. 2015; 132:2037–2099
- Krishman U, Takasuki S, Ivy DD Kerstein J, Calderbank M, Coleman E, Rosenzweig EB. Effectiveness and safety of inhaled treprostinil for the treatment of pulmonary hypertension in children. Am J Cardiol 2012: 110(11):1704-1709
- Kuch BA, Saville AL, DE Toledo JS, Inhaled Pulmonary Vasodilators: Are there indications within the PICU? Respir Care 2017: Vol 62 No 6: 678-698
- 1Manupipatpong K, 1Burdick-Will J, 1Diaz-Rodriguez N, 2Romer L, 2Coulson J, 1Wadia R 1 Johns Hopkins Children’s Center, Baltimore, MD, USA; 2 JHH A Review of Inhaled Epoprostenol (Flolan) Use in Children with Pulmonary Hypertension Admitted to the PICU
- Galie’ N, Barbera’ JA, Frost AE, et al; Initial use of anbrisentan plus tadalafil in pulmonary arterial hypertension N Engl J Med 2015; 373 (9):1-31
- https://pulmonaryhypertensionrn.com/wp-content/uploads/2013/03/Functional-Classification.jpg
Email newsroom@aarc.org with questions or comments, we’d love to hear from you.













