
RT educational programs are largely focused on the care and treatment of adults with respiratory conditions, and rightly so. After all, adults make up the lion’s share of people who need the services of a therapist.
But infants and children need RTs too, and many therapists get into the profession with the clear idea that this is where they want their careers to take them.
Jasmine Brown, MS, RRT, RRT-ACCS, COPD-Ed, CHSE, an associate professor and director of clinical education at Middle Georgia State University (MGA), had an experience earlier in her career that led her to the strong conviction that more therapists can and should get out of school with some solid bedside experience taking care of infants in particular.
“I was working in the ER and a teenage girl came in with severe abdominal/pelvic pain,” she recalled. ”Turns out she was pregnant and didn’t know it.” The girl ended up delivering the baby early, after having had zero prenatal care, and Brown felt like she was almost as unprepared as the astonished young woman herself. “Though I was NRP certified, I had no hands-on experience,” said Brown.
When she joined the faculty at MGA she decided to advocate for more neonatal training for her students. What started small when the program was still at the AS level has grown markedly, and the now four-year, entry-level BS degree program offers a full blown neonatal track that students can enroll in to acquire the kind of experience Brown herself was lacking when that teenaged girl came into the ER.
A team effort
Teri Miller, MEd, RRT, chair of the department of respiratory therapy at MGA, says Brown worked closely with other clinical instructors in the program to make the track a reality. “The design does several important things,” she said. “It gives an opportunity for a group of our students to explore, experientially, neonatal care in more depth, helping them to build their portfolio, and it serves as collaborative project between our program and our primary clinical sites, strengthening this relationship and serving the needs of each.”
Miller says the end result is a graduate who can make a smooth transition into a neonatal role upon graduation in hospitals that need more neo-peds RTs. “A win-win for all,” she said.
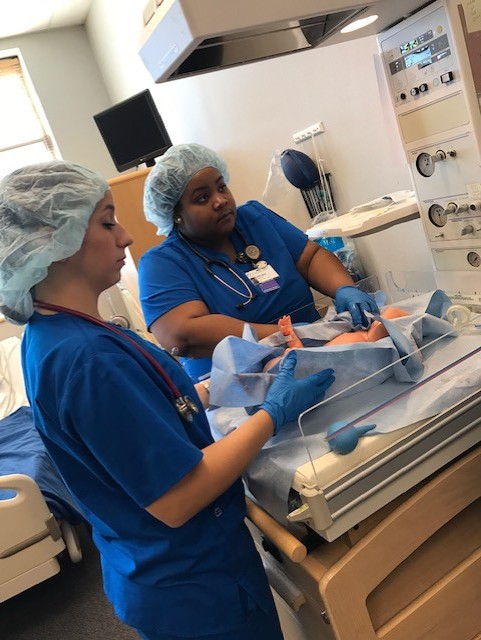
 The neonatal track includes a variety of high-risk scenarios. Jessica Brown takes part in a simulation session.
The neonatal track includes a variety of high-risk scenarios. Jessica Brown takes part in a simulation session.Brown agrees getting the track up and running was a team effort. She began the process by interviewing the program’s community partners to see where the need for neonatal RTs lie. From there she reached out to a local colleague, Sam Collier, then an RT who has since become a nurse practitioner. Collier was familiar with the training required to work in the NICU and offered to help her put the track together.
As the program began to take shape, Nancy Guyse, MSc, RRT, RRT-NPS, AE-C, an assistant professor at MGA, and part-time faculty member Jason Hunter, BS, RRT, RRT-NPS, got into the act as well.
Miller says the track fell right in with the Quality Enhancement Program (QEP) already underway at MGA too. “This program design was a perfect fit for this project,” she said. “We were able to associate it as a QEP project for our program and submit it to the university QEP team for approval, demonstrating how it would provide experiential learning beyond the curriculum and enhance student learning.”
Once the track received approval, they were able to apply for additional funding as well, and students could access additional content on service learning and community impact. The track has now become interdisciplinary too, with department of nursing faculty integrated into the mix.
“The result is a more realistic experience for the students, which helps build communication and collegiality,” said Miller.
Here’s how it works
Nancy Guyse, who serves as the primary neonatal track instructor, explains how the track is set up. “Our neonatal track consists of six to eight hours in the fall semester and 18 hours in the spring semester, with 24 to 26 hours total,” she said. In the past couple of years, two spots have been created for nursing students, upping the interdisciplinary appeal of the training.
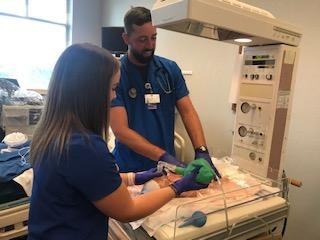
 Simulation training is a critical part of the program.
Simulation training is a critical part of the program.Content covered in the program is designed to reinforce NRP skills and develop knowledge in identifying and caring for common neonatal disease processes. “With support from our community partner Atrium Health Navicent, all respiratory therapy students, and the selected nursing students, earn their NRP certification,” she said. The hospital also provides STABLE certification to the neonatal track students, augmenting the NRP certification they will need to specialize in the care of neonates.
Guyse says the fall semester is devoted to discussion and hands-on experience, beginning with a conversation about what makes a pregnancy high risk and what to focus on when preparing for a high-risk delivery. “Once comfort is developed in preparation skills we move into discussions on the initial steps of stabilizing a neonate,” she continued.
Students practice everything from “catching” the neonate and starting a timer, to drying and stimulating the newborn, and clearing the airway. They learn how to monitor the devices involved and how to use resuscitation devices, including flow dependent and t-piece devices.
Assessment skills and the need for open communication among team members is part of the instruction as well.
“After each group completes the mini-simulation we all discuss these experiences and how they felt,” said Guyse.
Once students are comfortable with these aspects of care, they take part in high-risk scenarios that can range from placental abruption, lack of prenatal care, and suspected drug and alcohol use, to general pre-term delivery, pre-eclampsia, meconium aspiration, and maternal diabetes.
The fall semester draws to a close with sessions on APGAR scoring, intubation, surfactant administration, and a full simulation, if time permits.
The spring semester is focused on hands-on experience, with the first three sessions devoted to simulations. Typically, continued Guyse, they run four to six full simulations, including a pre-brief and debrief for each. Students are encouraged to take on leadership roles during each of the simulations.
“After the first three sessions, the nursing students complete their experience within the neonatal track and the respiratory therapy students shift their focus to respiratory equipment utilized within the neonatal population,” continued Guyse. That begins with a session on HFNC, bCPAP, and NIV, and is followed by a session on mechanical ventilation of the neonate.
“Our final session is dedicated to HFOV and nitric oxide,” she said. Once again, Atrium Health Navicent has stepped up to assist, providing the space and equipment for students to gain the hands-on experience they will need to work in this setting, not to mention NICU clinical hours for each student in the track over an eight week period.
“With these dedicated clinical hours our neonatal track students are offered a unique experience in developing confidence in caring for our neonatal population,” said Guyse.
Rodney Cooper, BS, RRT, assistant vice president of respiratory services and neurodiagnostics at Atrium Health Navicent, sings the track’s praises. “With the shortage of neonatal respiratory therapists today, the neonatal respiratory track program that MGA and Atrium Health Navicent collaborate on serves to help with the neonatal care for the region,” he said. “It helps to get them better prepared to take care of this population when they graduate and helps to fill a much needed demand for respiratory therapists in neonatal care.”
Students give it high marks
Jasmine Brown believes the neonatal track allows students to build the confidence they will need to step out of adult care into the world of infants and children and notes some of the students who have gone through the program have already earned their NPS credential from the NBRC as well.
“This is good for our profession,” she said. “Specialty tracks can help meet the needs of community partners by filling the gaps in the local market.”
Students who have completed the track give it high marks. “Participating in this program allowed me to work in the NICU immediately after graduating,” said Aaron Fowler, BS, RRT, RRT-NPS. “I quickly gained knowledge and experience others in my class were not exposed to. Now, three years later, I am working at a children’s hospital in the NICU and PICU as an RT, charge therapist, and ECMO specialist.”
 Thanks to the experience he received in the neonatal track, Aaron Fowler was able to step right into the NICU after graduation.
Thanks to the experience he received in the neonatal track, Aaron Fowler was able to step right into the NICU after graduation.Rhianon Mangan, RRT, says the neonatal track provided hands-on experience working in the NICU alongside experienced RTs, something that made her more comfortable with the idea of caring for such tiny and vulnerable infants. “Most students only get about two weeks to rotate through the NICU,” she said. “As a student, I was able to work in Level II and III units taking care of babies as small as 500 grams, work with oscillators and bubble CPAPs, and attend high risk deliveries.”
She credits her professors in the program for going the extra mile and she’s thankful that she was able to take advantage of the experience. “This is a special population, and as a respiratory therapist, you have so many opportunities to impact the lives of the patients and their families with your specialized skill set and compassion,” she said.
Jessica Brown, BS, RRT, is also “beyond thankful” for the chance she had to participate in the track during her time at MGA. “I think that it’s safe to say that participating in this program allowed me the opportunity to work in a Level IV NICU post-graduation at one of the best children’s hospitals in the area, with ease!” she said.
Four great tips
The neonatal track at Middle Georgia is fairly unique among respiratory care programs, but Jasmine Brown, Teri Miller, and Nancy Guyse believe it’s something other RT programs could implement as well. Guyse offers these four tips to any program that might be considering a similar track —
Start small. You don’t need your own high-fidelity baby. We started with a couple of students, a couple of non-simulation dolls, and a community partner, Houston Healthcare, who graciously provided their high-fidelity baby for a couple of simulation sessions.
No additional work for the students. Each respiratory therapy program has unique neonatal/pediatric courses. Develop your neonatal program from what is already built into your program. This will take away the need to provide extra work for the neonatal track students.
Provide a valuable opportunity. When students learn we provide this unique program, but there are only a specific number of seats, they know they need to work for this valuable opportunity. However, it’s important for students to understand selection comes from not just GPA and grades in the neonatal/pediatric courses, but also desire.
Seek support. One or two people within a program do not have to do it all. We sought support from our community partners, our clinical instructors, and now our nursing neonatal track liaison.
Teri Miller says she is tremendously proud of the work that her faculty and their community partners have done to extend the experiential education of MGA students into neonatal care. “By offering such specialty tracks, we give students the opportunity to connect with experienced practitioners who are passionate, and develop skills that are marketable for their future,” she said. “I hope to see the development of similar programs for other specialty areas in our future.”
Email newsroom@aarc.org with questions or comments, we’d love to hear from you.















