Jerry Krishnan, MD, PhD, Builds Teams to Battle Lung Disease
As a respiratory therapist, you no doubt prefer to work with physicians who take your ideas and concerns into account when caring for patients or making decisions regarding the kind of care patients should receive.
Ellen Becker, PhD, RRT, RRT-NPS, RPFT, FAARC, has a great story to tell about this year’s Jimmy A. Young Medalist, Jerry Krishnan, MD, PhD, that speaks to that need.
“At an organizational meeting for a CHICAGO Plan grant, there were approximately 45 stakeholders representing varied disciplines present either in the room or on the phone,” said Dr. Becker, a professor at Rush University Medical Center in Chicago, IL. “The meeting lasted 45 minutes.”
Dr. Krishnan was leading the meeting, but with that many people involved, you would think very few would leave feeling totally heard. Dr. Becker says think again.
“Dr. Krishnan skillfully found a way to get the opinions of everyone while making each individual feel valued and highlighting their skills,” she said. “I have never seen someone move along the discussion in such a large a group while not rushing individuals, but including all within the designated time frame.”
Making his way to pulmonary medicine
That spirit of inclusion has pervaded Dr. Krishnan’s career. Over the years he has collaborated not just with other physicians, but with RTs, nurses, and other members of the health care team as well.
“I have always enjoyed working in multidisciplinary teams,” said Dr. Krishnan. “For example, when I worked in the intensive care unit, I found the morning multidisciplinary rounds extremely helpful — each member of the team would offer their assessment and recommendations, and together we’d make a plan of care.”
 Jerry Krishnan, second from the left, took part in a day trip to the U.S. capital in November of 2017 to advocate for research funding to prevent and treat COPD.
Jerry Krishnan, second from the left, took part in a day trip to the U.S. capital in November of 2017 to advocate for research funding to prevent and treat COPD.His path to pulmonology, however, wasn’t a given.
Dr. Krishnan was born in India, where he lived until he was five years old. From there, the family spent five years in Algeria, then pulled up stakes again and made their way to Canada. As he was getting ready to start high school, they moved to Houston, TX, where he graduated high school and enrolled in the University of Texas at Austin for his undergraduate degree. He went on to get his medical degree from Baylor College of Medicine in Houston.
“In college, I was influenced by my peers and spent some time in an emergency department and intensive care unit as a volunteer,” he said. ”I was struck by advances in medicine and what they could do to bring comfort to people in need.”
When he got to medical school, though, he really wanted to become an orthopedic surgeon — until he realized he might be not be tall enough to do the job.
It wasn’t until he was doing his residency at Johns Hopkins in Baltimore, where he also earned his PhD in clinical investigation, that pulmonary medicine piqued his interest. “I enjoyed working with pulmonary/critical care medicine physicians, including Drs. Roy Brower, Sean Gaine, Robert Wise, and Peter Terry,” he said. “I realized that helping people breathe was my calling.”
Enter the Windy City
After about five years working as an assistant professor at Hopkins, Dr. Krishnan made the last big move of his life, to Chicago, IL, teaching first at the University of Chicago and then at the University of Illinois at Chicago, where he remains today, serving as a professor of medicine and public health and associate vice chancellor for population health and executive director of the Institute for Healthcare Delivery Design.
For Dr. Krishnan, the academic setting has afforded the chance to serve as a clinician, to learn from others, and to make advances in care. “Academic medicine also helps me to give back — to train the next generation. And to learn from them,” he said.
He learns something from every patient he treats as well, including how to make a diagnosis, how to co-develop a management plan, how to use effective communication, and how to employ empathy when prioritizing options for care.
He credits Drs. Roy Brower, Cindy Rand, Jon Samet, and Robert Wise for mentoring him in the ways of research, and emphasizes that his colleagues outside of medicine are important to him too, particularly respiratory therapists. “My first interactions with respiratory therapists were in the intensive care unit — I relied on them to help me understand what we could do to ‘liberate’ patients from mechanical ventilation,” he said.
Over the past 15 years, that relationship has moved to the outpatient setting, where he has worked with therapists to evaluate patients for home oxygen. “RTs taught me what I know about the use of home oxygen — not only how the various types of equipment work, but also how to prescribe home oxygen,” he said. ”It was this work that helped me learn about the limitations of home oxygen equipment and the limitations of reimbursement policies for home oxygen equipment.”
He has made home oxygen one of his main areas of study as a result. “Our patients deserve better,” said Dr. Krishnan. ”I am collaborating with RTs to find better solutions. In short, I am being educated by RTs!”
A gifted collaborator and leader
David Vines, PhD, RRT, FAARC, FCCP, who serves as an associate professor and program director of respiratory care at Rush University, first met Dr. Krishnan at an ATS meeting about ten years ago. That initial conversation blossomed into more discussions when they returned to Chicago and the two worked together on the Peer-Led O2 Infoline for patients and Caregivers (“PELICAN”) and the Home Oxygen Evaluation by Respiratory Therapists in Patients Hospitalized for COPD Exacerbations (“RIsOTTO”) studies.
 A group photo of University of Illinois Chicago and University of Wisconsin Madison members of The Great Lakes PrecISE Partnership to develop a personalized medicine approach to the treatment of severe asthma. That’s Dr. Krishnan at the top left.
A group photo of University of Illinois Chicago and University of Wisconsin Madison members of The Great Lakes PrecISE Partnership to develop a personalized medicine approach to the treatment of severe asthma. That’s Dr. Krishnan at the top left.“Dr. Krishnan is a gifted collaborator and leader,” said Dr. Vines. “He has worked tirelessly to improve the lives of patients with chronic lung disease and improve access to acute care as well as services needed in their homes. Dr. Krishnan sees a key role for respiratory therapists in COPD disease management regarding long-term oxygen therapy, aerosol device education, and pulmonary rehabilitation.”
Sam Giordano, MBA, RRT, FAARC, long-time AARC executive director and currently interim executive director for the Association, agrees. “Dr. Krishnan serves as one of the best, most effective, advocates for our patients, but also for those who serve them, especially physicians, respiratory therapists, nurses, and others,” he said. “His efforts to improve access to needed services for home patients, such as supplemental oxygen, has helped to better position patients to more effectively manage their chronic lung disease and improve their respiratory quality of life. He is a difference maker!”
Ellen Becker, who met Dr. Krishnan when she and her colleagues reached out to him for help with a CMS grant for health care innovation, believes his willingness to embrace RTs as colleagues is priceless.
“A significant challenge throughout the history of respiratory care is gaining professional recognition,” she said. “Dr. Krishnan regularly elevates respiratory therapists and assures that they have a seat at the table. His mentorship and inclusion are critical for our research development — the ability to define our roles and the future of our profession.”
Putting things into perspective
Dr. Krishnan has collaborated with RTs, nurses, and other physicians on numerous studies, but one that stands out for him is the 2004 trial that was aimed at gauging the effectiveness of protocol directed care in the discontinuation of mechanical ventilation in the ICU. “The study was led by Dr. Henry Fessler and was designed to help us understand whether weaning protocols shown to be effective in one setting offer benefits in other settings,” he said.
For him, the process of designing, implementing, and writing the study results was as important as the study findings, which showed in this case that weaning by nursing and respiratory therapy according to the protocol did not reduce duration of mechanical ventilation, length of stay, or mortality when compared to weaning by physicians.
That may seem a disappointing result to RTs, but Dr. Krishnan believes everyone learned some important lessons that would serve them well going forward. Specifically, the team ended up speculating that the lack of benefit seen for the protocol stemmed from the fact that there were high levels of physician staffing in their intensivist-run, closed ICU — which was already consistently using a template on rounds to promote daily discussion of mechanical ventilation on each patient.
“In other words,” he said, “context matters.”
Bringing research into the real world
In addition to mechanical ventilation and home oxygen, Dr. Krishnan has a significant interest in asthma and COPD.
When it comes to asthma, the connection is personal — he has long suffered from the condition himself. “There is much work to do to more fully understand the biologic mechanisms that contribute to these airway disorders,” he said. “We also need more effective therapies and, most importantly, proven-effective prevention strategies.”
One shortcoming he would like to see resolved is the dearth of research studies on asthma and COPD that are conducted in real world settings.
“Much of the evidence base for the management of asthma and COPD come from studies conducted in research settings — not real-world clinical and community settings that include substantially more heterogeneity in terms of subtypes of asthma or COPD, comorbidities that complicate these conditions, and patient-level and clinician-level behaviors,” said Dr. Krishnan.
Studies in research settings rarely account for the perspectives of policymakers and payers either, and he believes those factors contribute to a limited uptake of research evidence into day-to-day practice. That’s why, in recent years, he has focused considerable effort on how health care systems can work more closely with stakeholders to effect real world solutions and implement them in local communities.
That feeds right in to his latest initiative, which is focused on long-COVID and how the public health burden caused by the pandemic can be lessened and health inequities can be resolved.
Other projects dear to his heart
Dealing with health issues in the real world has been key to another of Dr. Krishnan’s pet projects, the COPD Outcomes-based Network for Clinical Effectiveness and Research Translation, or “CONCERT.” Funded by the Agency for Healthcare Research and Quality, the network published a study in 2013 aimed at developing methodologies to prioritize research topics for real world COPD research.
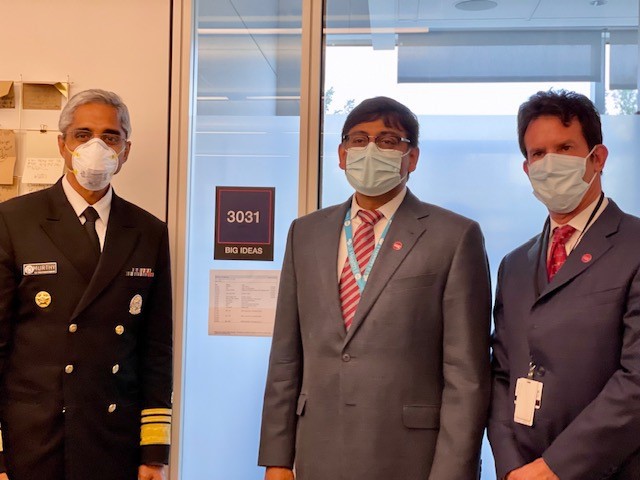 Surgeon General Vivek Murthy, left, with Dr. Krishnan, center, and Dr. Ian Jasenof during a meeting to discuss burnout during year two of the pandemic.
Surgeon General Vivek Murthy, left, with Dr. Krishnan, center, and Dr. Ian Jasenof during a meeting to discuss burnout during year two of the pandemic.“Over a two-year period, we met with representatives of 54 stakeholder groups via teleconferences and in-person workshops using a modified Delphi approach to facilitate discussions and consensus building,” said Dr. Krishnan. ”This study helped us to understand how to build consensus — and many of the studies I am conducting are linked directly to these stakeholder priorities.”
Right now, he is actively engaged in a study funded by the American Lung Association in conjunction with a range of other investigators called “INSPIRE COPD.” The goal is to develop a shared decision-making tool that can facilitate communication between patients and their providers regarding the use and discontinuation of home oxygen.
“Can’t wait to see what I learn from this study,” said Dr. Krishnan.
Another initiative that has been especially important to him during his career is the ATS Methods in Epidemiology, Clinical, and Operations Research Program (MECOR), which, since 1994, has focused on building lung disease research capacity in low and middle income countries. So far, more than 2,500 individuals have been trained by the MECOR faculty.
“The ATS MECOR Program was co-developed by Sonia Buist, MD, and has helped not only trainees in gaining new skills, but has also helped the faculty to learn from trainees all over the world,” he said.
He is proud of his involvement in the FDA’s Pulmonary-Allergy Drugs Advisory Committee, the NIH/NHLBI Clinical Trials Review Committee, and the Global Initiative for Asthma as well, noting that all of these opportunities facilitated his growth as a scientist. “The work on these committees has also helped me to learn how to make decisions when there is no single right answer,” he said.
Collaborating with the AARC
Dr. Krishnan has collaborated with the AARC on several projects too, including the ATS guidelines for home oxygen that were published just last year. He also helped the Association devise a survey of the AARC membership regarding their involvement in the provision of home oxygen, which highlighted the role RTs could play in hospital-to-home transitions.
“I am now working with some members of the AARC to consider how respiratory therapists can be engaged in acute hospital-at-home programs that are increasingly used in the U.S.,” he said “The AARC is a natural partner for pulmonologists interested
in re-designing care models to better serve the needs of people with respiratory disorders.”
Dr. Krishnan has special thanks for Sam Giordano, Thomas Kallstrom, MBA, RRT, FAARC, Joseph Lewarski, MHA, RRT, FAARC, and David Vines for introducing him to the AARC and collaborating with him on so many efforts.
A well-deserved honor
What did Dr. Krishnan think where he heard he would be receiving this year’s Jimmy A. Young Medal. He summed it up pretty simply: “Shock. Surprise. Appreciation.”
Sam Giordano believes it’s an honor well deserved.
“Dr. Krishnan has devoted his entire career to helping patients with lung diseases through his extraordinary research efforts, educating professionals such as respiratory therapists, physicians, nurses, and family caregivers,” he said. “He continues to demonstrate a wide interest in collaborating with both patient advocacy groups, as well as the professional provider communities, while continuing to drive thoughtful changes based on effectiveness research and advocacy.”
Email newsroom@aarc.org with questions or comments, we’d love to hear from you.














