Chronic obstructive pulmonary disease (COPD) is listed as the third leading cause of death globally.1 COPD is characterized by limitations in expiratory airflow, emphysematous destruction of the lungs, chronic bronchitis, and chronic inflammation within the lung tissue. Although COPD prevalence continues to rise, strategies for prevention, treatment, and management of the disease are limited.
The two most common clinical conditions of COPD include chronic bronchitis and emphysema. Chronic bronchitis is the inflammation of bronchial tubes leading to the narrowing of the small airways, which carry air in and out the air sacs (alveoli) in the lungs. Emphysema, also known as parenchymal destruction, is characterized by abnormal permanent enlargement of air spaces distal to the terminal bronchiole, resulting in a loss of alveolar attachment and a decrease in the elasticity of the lungs. These changes keep the lungs from remaining open during expiration, limit airflow in the airway, reduce expiratory output, and cause dyspnea, a common symptom of difficult breathing. In addition to emphysema, patients with COPD often experience chronic bronchitis consequent to mucus accumulation in the lung. The mucus is mainly produced by goblet cells, which act as the first line of defense for the respiratory tract and interact with the immune system. Epithelial damage due to COPD-associated chronic inflammation and loss of lung elasticity cause difficulties in clearing the airway of mucus. Therefore, the accumulation of the mucus and an unproductive cough due to respiratory muscle weakness exacerbate symptoms of chronic bronchitis. The clinician may seek similar or different care plans in caring for chronic bronchitis and emphysema; however, airflow is the central issue. Therefore, the use of an evidence-based strategy is best.
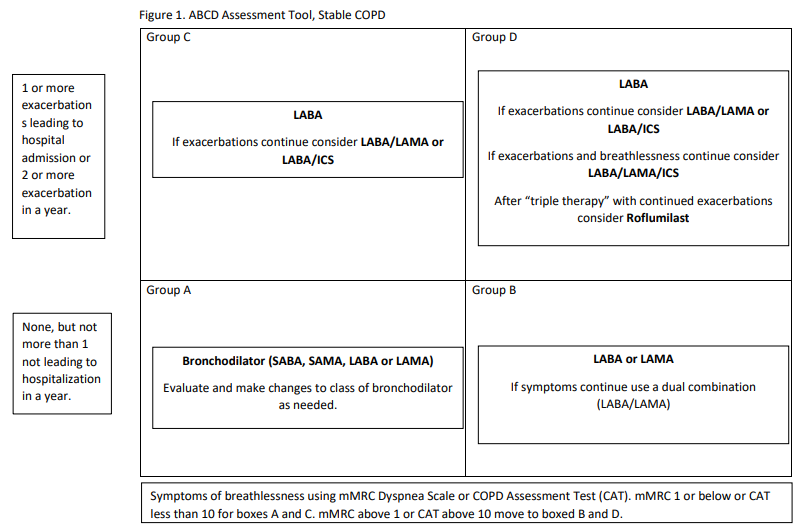
This review will cover the existing classes of drugs including, β2-agonists, anticholinergic agents, corticosteroids, and PDE4 selective inhibitors. In evaluating COPD for treatment, the best strategy is to use information from GOLD COPD.2 In Figure 1, you will find the ABCD assessment tool for the treatment of stable COPD.
Beta Agonists
The main indication for using a beta-adrenergic bronchodilator (Table 1) is to reverse airflow obstruction. These agents treat asthma, bronchitis, bronchiectasis, cystic fibrosis, and chronic obstructive pulmonary disease (COPD). Additionally, beta-adrenergic agents containing alpha receptor properties may be used to treat upper airway conditions such as stridor, croup, and epiglottitis.3
Epinephrine and racemic epinephrine are often used for their alpha-receptor effects. These agents possess a vasoconstricting effect to reduce airway swelling after extubation (stridor), croup, and epiglottitis. Additionally, these agents can cause an increase in myocardial contractility and heart rate due to beta1-receptor stimulation. These agents are available over-the-counter and marketed to individuals with breathing issues. However, Epinephrine and racemic epinephrine should not be used to treat COPD, as many newer agents with fewer side effects exist.
Short-acting beta-agonists (SABAs) such as albuterol and levalbuterol are used to reverse airflow obstruction during acute episodes of bronchoconstriction. They are beta-2 receptor-specific agents producing fewer side effects.
Long-acting beta agents (LABAs) such as salmeterol, formoterol, arformoterol, indacaterol, olodaterol, and vilanterol are indicated for managing COPD. In addition, many LABAs can be found in combination with other agents such as glucocorticoids and anticholinergic agents.
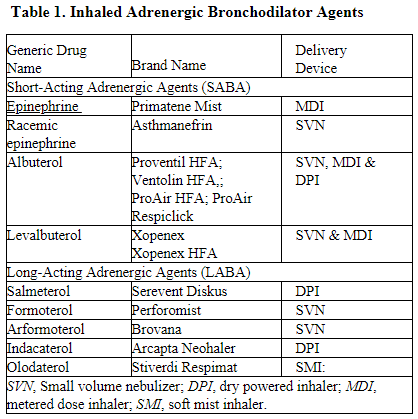
Based on the GOLD COPD strategy and using the ABCD assessment tool, any bronchodilator can be used as first-line management based on dyspnea and exacerbation history for stable COPD. The clinician should evaluate the effect of the agent and make changes to other bronchodilators such as a LABA or an anticholinergic bronchodilator if determined. During exacerbation of COPD SABA, anticholinergic bronchodilators, and glucocorticoids are first-line agents for COPD exacerbation.
Anticholinergic Bronchodilators
Bronchodilation can also be achieved through a blockade of cholinergic (muscarinic) receptors. The muscarinic 3 receptor is the main receptor responsible for bronchoconstriction on the airway smooth muscle. The blockade of this receptor creates bronchodilation if active bronchoconstriction is present. These agents (Table 2) are often referred to as muscarinic antagonists and categorized as a short-acting muscarinic antagonist (SAMA) or a long-acting muscarinic antagonist (LAMA).4
Anticholinergic bronchodilators are used mainly in the treatment of COPD and as add-on therapy in asthma. Using the ABCD assessment tool, LAMAs are useful for treating all levels of stable COPD. Although research does not demonstrate that a LAMA is superior to LABA, dyspnea should be evaluated and changes made based on breathlessness. If more dyspnea persists, the use of LAMA and LABA is dictated as described in the next section and as noted in Group B or C of Figure 1. However, a combination of medication, including corticosteroids, may be necessary based on exacerbation and dyspnea.
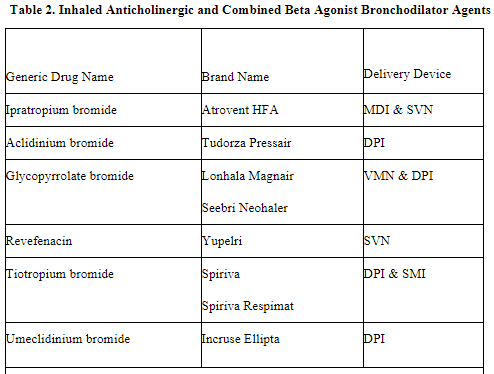
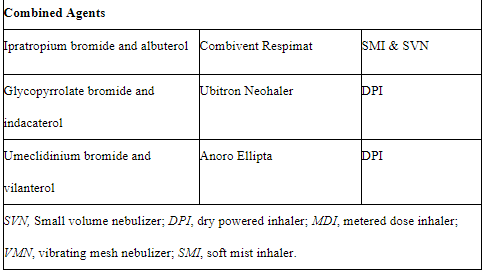
Combined Anticholinergic and Beta-Agonist Bronchodilators
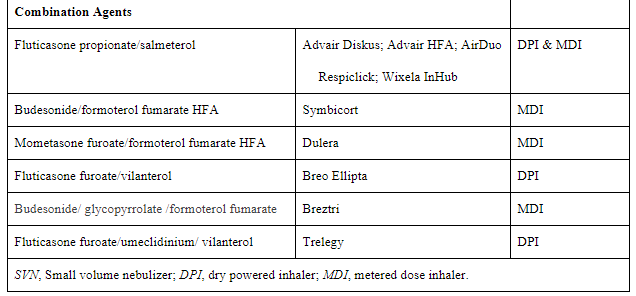
The combination of an anticholinergic and beta-agonist may be indicated for those with COPD. Depending on symptoms, short or long-acting agents may be used. Combination bronchodilators, especially LABA/LAMA, demonstrate dual bronchodilation that may be more beneficial than monotherapies or other inhaled treatments (Table 2).4 The combination of LABA/LAMA improves lung function and outcomes in patients with COPD, especially patients with low exacerbation rates, as seen in Groups B and C in figure 1. The use of triple combination in a fixed-dose termed “triple therapy” is available to patients that continue to experience increased exacerbations while receiving LABA/LAMA therapy. Triple therapy provides the addition of an inhaled corticosteroid.
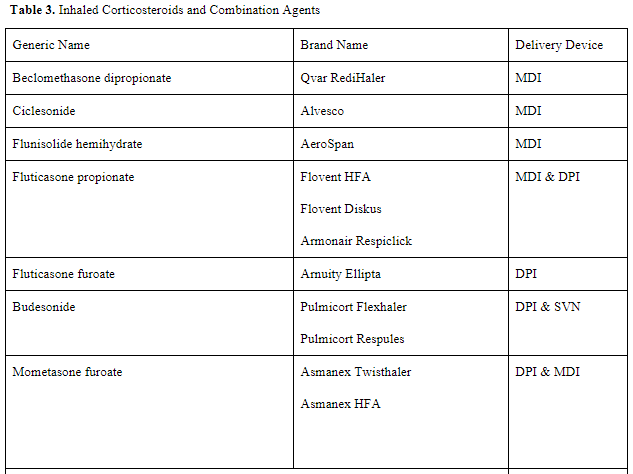
Inhaled Corticosteroids
Corticosteroids are hormones produced by the adrenal cortex. They produce an anti-inflammatory effect and assist in the regulation of metabolic functions in the body. Inhaled corticosteroids are commonly combined with bronchodilators. Although inhaled agents may be used in managing stable COPD, oral corticosteroids are used in COPD exacerbations with SABAs to assist in restoring responsiveness and increase the availability of beta receptors. Corticosteroid use can lead to immune response making patients more susceptible to infections, such as pneumonia.5
Roflumilast
Roflumilast is a selective phosphodiesterase 4 (PDE4) inhibitor used to reduce the risk of exacerbations in patients with severe COPD. The starting dose of roflumilast is 250 mcg tablet daily for the first four weeks, then 500 mcg daily. This agent is not a bronchodilator and should not be used for acute treatment. This agent is an add-on in Group D seen in Figure 1. Patients experiencing more exacerbations in those with chronic bronchitis and a reduction of flow below 50% of their FEV1.2
Conclusion
When treating acute COPD exacerbations, all medication used to treat acute airflow limitations should be considered. When working with stable COPD patients, the GOLD COPD strategy can be used as a starting point based on clinical breathlessness and exacerbation history. In caring for any patient, the clinician should also consider patient preference, delivery device, and cost.
References
- World Health Organization (WHO), Leading cause of death December 9, 2020 https://who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death
- Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. 2020. Available from: https://goldcopd.org/wp-content/uploads/2019/12/GOLD-2020-FINAL-ver1.2-03Dec19_WMV.pdf. Accessed September 6, 2021.
- Gardenhire DS. Adrenergic Bronchodilators. In: Gardenhire DS, editor. Rau’s Respiratory Care Pharmacology, 10th edition. St. Louis, MO: Elsevier; 2020:90-111.
- Gardenhire DS. Anticholinergic Bronchodilators. In: Gardenhire DS, editor. Rau’s Respiratory Care Pharmacology, 10th edition. St. Louis, MO: Elsevier; 2020:112-126.
- Gardenhire DS. Corticosteroids in Respiratory Care. In: Gardenhire DS, editor. Rau’s Respiratory Care Pharmacology, 10th edition. St. Louis, MO: Elsevier; 2020:168-185.
Email newsroom@aarc.org with questions or comments, we’d love to hear from you.