Fall/Winter 2016 Leadership & Management Section Bulletin
Fall 2015 Leadership & Management Bulletin
Roger L. Berg, PhD, DSc, RRT-NPS
RT Instructor
American Career College
Ontario, CA
rpberg2@verizon.net
Cheryl Hoerr, MBA, RRT, FAARC
Director, Respiratory Therapy
Phelps County Regional Medical Center
1000 W. Tenth Street
Rolla, MO 65401
choerr@pcrmc.com
573-458-7642
Bill D. Cohagen, MSHCA, RRT, FAARC
In this issue:
• Cost Reduction vs. Revenue Generation
Jeffrey Davis, BS, RRT
- How to (Hopefully) Avoid Catastrophes: Valuable Tips on Hiring Great People
Joy Hargett, MBA, RRT - What’s on Your Mind? An AARConnect Discussion Forum Survey
John S. Rinck, MM, RRT-NPS, CPFT - Section Connection
Cost Reduction vs. Revenue Generation
Jeffrey Davis, BS, RRT
Director of Respiratory Care and Pulmonary Function
UCLA Ronald Reagan Medical Center, Los Angeles, CA
During these difficult economic times, hospitals, just like other institutions, must gain or maintain a competitive market share. Whether the hospital is considered not-for-profit or is corporate owned, the mission remains the same: provide superior, cost effective patient care.
While the senior administrative team makes decisions for the hospital, individual department directors must determine the ideal plan for their department. Are cost cutting initiatives the direction to take, should aggressive revenue generation plans be implemented, or is the answer a combination of the two? Finding the solution may lie in the four-step process of strategic planning.
So, what are they thinking?
Implementing your own strategic planning initiative can help determine the correct plan of action for your department. Should your goals be the same as your CEO’s? This question was posed to me, along with a group of other directors, by my CEO back in 2006. I was a novice department director at the time, and the answer seemed too easy to be right, so I bit my tongue and kept quiet. (The answer later.)
In a recent interview with several CEOs, it was anecdotally stated that budget allocation will shift in part toward revenue generation. If cost-cutting measures are to be implemented, a measurable return on investment must be demonstrated.1 One possible way to achieve this is to provide case studies to show how other departments have implemented successful cost cutting measures.
Strategic planning
The Six Sigma organization recommends what they call the “DMAIC” methodology of strategic planning to determine whether a revenue generating or cost reduction project will work. It is important to understand that it is the service the customer receives, and their impression of the quality of that service, rather than performance based on measurable data that matters the most.2
Using the DMAIC methodology, you will —
Define the objective to achieve higher revenues. This may be done by merely speaking with your employees. They may have the best ideas, which are lying dormant because you simply didn’t ask.
Measure key aspects of services within your department. Are waiting times long for certain procedures? Are there services lacking in your community? Certain programs such as pulmonary rehabilitation have collapsed in communities due to the failure to generate revenue, yet an important aspect may have been forgotten. Revenue may come from unsuspected sources by implementing a community service that otherwise is not a big money maker. Physicians may be more inclined to admit their patients to your facility because of services provided that other facilities do not provide.
Analyze the decision and then Identify the action plans required to implement the program.
Finally, once the changes and programs are put into place, the Control phase makes sure you sustain the efforts and achieve the expected outputs.2
What choice do you make?
Strategic planning gives you a process to follow to determine the direction you need to take in your department. Analysts agree that revenue generation and cost reduction programs work, and with correct planning either program can be successful. Rust et al., however, found that there is little evidence “for the effectiveness of attempting both revenue expansion and cost reduction simultaneously, and some of what little empirical and theoretical literature is available suggests that emphasizing both simultaneously may not work.”3
Rust and his team go on to discuss how, generally speaking, companies that implement revenue generating programs generally do better than companies that focus on cost reduction, but both efforts yield better results than attempting to implement both revenue generating programs and cost reduction efforts at the same time.3
How do you choose revenue generation? Respiratory therapy departments are cost centers. They have been for years. But there are still ways we can provide services to the hospital that are cost-reducing services. Can you compete with your competitors? What similar services do the other hospitals in your community provide that your department can improve upon and provide better, cheaper, or faster?
Find a product that is poorly served in your community. Talk with the providers in your community. What services do they find lacking for their patients? Is it a slow turnaround for pulmonary function results, or a pulmonary rehabilitation program that underserves the community? Work “smarter, not harder.” Having a well-educated staff that is committed to the department helps to provide exemplary customer service, and this brings the customers back.
How do you choose cost reduction? Again, it is time to look at the services you provide. Are your ABG machines old and outdated? Do you have a disposable purchasing contract with a provider? This usually entails the no cost delivery of capital equipment with a contract over time to purchase the disposable supplies at a specific price until the cost of that capital equipment is covered. Ventilator companies, pulse oximetry companies, and ABG machine companies all provide similar services, and surprisingly, you may find you are actually reducing cost by bringing in new capital equipment. This is where your research and hard work come in to play, because a positive ROI is important for your CEO to sign off on the project.
The answer is simple
So, should your goals be the same as your CEO’s? This simple question has an even simpler answer. Yes. Emphatically, yes! Know the direction the hospital is going. Know the goals of your CEO. Know your department and the community you serve. Revenue and increased cash flow occur when you provide a product that your customers cannot get easier and cheaper somewhere else. Make your department invaluable to the hospital. Provide services otherwise unavailable in the community. Complete your strategic planning in advance of the capital budgeting process, and be sure to provide your CEO with a positive ROI.
Most importantly, know your senior leadership. Know their plans in both the short-term and the long-term. Make sure your goals match the goals of your CEO.
References
- Rocket Watcher. October 30, 2008. Notes from a conversation with a dozen CIO’s. http://rocketwatcher.com.
- Six Sigma Training for Healthcare. October 28, 2008. Six Sigma Training Certification. http://sixsigmaonline.org/articlelive/articles/688/1.
- Rust R, Moorman C, Dickson P. Getting return on quality: revenue expansion, cost reduction, or both? Journal of Marketing 2002;66:7.
How to (Hopefully) Avoid Catastrophes: Valuable Tips on Hiring Great People
Joy Hargett, MBA, RRT
Manager, Respiratory Care, Baylor St. Luke’s Medical Center, Houston, Texas
Hiring is an arduous process, but it’s something all employers must do. As department leaders, we may feel we have just gotten the right mixture of talent in our department and then BAM, something happens — employees have life -changing events affecting their ability to come to work when we need them. They want a job closer to home because of family or a lengthy commute. They have an opportunity to advance their careers. They want to cut back their hours. Someone has gotten sick and they are now the primary caregiver. They have scheduling demands or need to move to another shift because of personal reasons. The list goes on and on.
Or, you could be experiencing growth in your market. You are adding services or beds and need more qualified people.
So, here you are again, trying to recruit the right person to fill an open position. What do you do to make the process smoother and end with the perfect employee?
First of all, you must realize you won’t end up with the perfect person — that’s because no one is perfect! Each and every one of us has flaws and we all have a personal life. So, since perfect is not available, we need to do everything we can find the best candidate possible.
Three things to consider
Whether or not you have an abundance of candidates, hiring a new employee is a very important part of a leader’s job. You want to find someone who is not only able to do the job but is also willing to do the job. Working in the health care environment does require sacrifices. Typically, health care institutions don’t close up at the end of the day so everyone can go home. Most health care institutions are open 24/7/365. And finding employees who accept those conditions is often difficult, again, due to the many factors listed at the beginning of this article.
So, how do you determine whether an applicant is truly suitable for your organization? To be successful, do some prep work before you meet with a candidate.
First of all, perform a needs assessment. Do you need a seasoned therapist with years of critical care experience or can you take on a new graduate with limited skills? The answer to the question may not be the same each time you are looking to hire, but it’s always something to keep in mind.
Second, what are the needs of the organization or department? Is the organization adding a particular type of service that requires specialty skills of its practitioners? Is your department adding a new service that will require more new skills?
Next, we all need to look at succession planning. How do we plan for the future? Eventually, all employees will leave their place of employment. So, one key is to focus on the type of employees that are needed to fill in the gaps as people naturally depart the work force.
Tips on reviewing resumes and conducting interviews
As leaders, we all try to review applications thoroughly, but here are some things that might be overlooked —
- When reviewing a resume or job application, look for gaps in employment dates or between school and employment. There may be legitimate reasons for the gaps, but it is always good to ask the candidate why they weren’t working during this time.
- Ask lots of questions about comparative experience. Some new graduates may not have worked in a hospital or health care environment, but questions can be tailored to their other experiences. Questions relating to customer service and helping people can be gleaned from any past work history or even involvement in high school or college activities, such as sports or volunteer work.
- Ask open-ended questions — questions that require more than a yes or no answer. It’s a good way to judge an applicant’s communication skills. Questions that start with “Tell me about . . .” should give the interviewer an idea of the applicant’s communication skills.
- There are some questions that employers legally can’t ask. If you are unsure of what is acceptable, work with your HR department. However, there are ways to uncover answers to questions you really need to ask. Just ask the question a bit differently. For example, employers want to know if an applicant will come to work when scheduled and will be on time. We usually can’t ask where someone lives or how they will get to work, but we can ask questions that get the answer we are seeking. For example, one question about time management may be something like, “Our shift starts at 6 a.m. Do you foresee any reason why you can’t be at work at that time?” If they say they have a problem with the start time, ask them to explain why, so you can fully evaluate their situation and compare it to your needs.
- When possible, involve other department members in the interviewing process and then compare notes. Look for consistencies between answers. Each interviewer will have a different perspective on the applicant, which might be useful if several candidates are vying for one position.
Key factors in evaluating applicants
Several factors should come into play when you’re considering whether or not an applicant is right for your department –
- Fit — does this candidate fit with the current culture? All departments and institutions have cultures, which are created by the organization and the employees. Will this candidate fit in with the organizational goals and their co-workers? Fit is a very important quality that many leaders overlook during the evaluation of job candidates.
- How will the culture change with the addition of this new employee and is that good for the organization? Organizational cultures are dynamic and change to some extent as new members join the team — maybe only slightly, but it will change. So, does this candidate offer positive attributes that can help drive the team forward into success? Or, does this candidate offer challenges that might not be readily accepted by the team or be in line with the strategic goals of the organization?
- Energy and attitude — is the applicant generally interested in caring for people? Does he seem to be a positive person? Does she show compassion for others?
- Do they offer something new to the organization? Unless the job is very specific, look at what the candidate can bring to the table. What are their skills? Can they make the team a better team?
- Can they be trained on what the organization needs them to do?
- Do they have the appropriate qualifications and experience?
We can also look at some lessons from other industries. Search the Internet for employment websites and you will find what other employers are seeking in potential employees. Here is a quote from Steve Wynn, CEO and chairman of Wynn Resorts, regarding the type of employees his organization seeks.
“We want someone who is genuinely interested in the fine art of making people happy. At Wynn, the guest experience is everything, and if you have the ambition to make our guests happy, then you know what? You have the same exact ambition we do.”1
While we don’t all work for a 5 Star resort in the heart of Las Vegas, there is a take-away from the message above. Health care organizations need employees who not only can take care of patients, but also genuinely enjoy their job and their role as caregivers. If people like their jobs, it shows in their words and actions. We should all strive to make our patients and their families happy and help them feel good about the care they are receiving. Not only can this help to improve patient outcomes, it also improves HCAHPS scores as well as the patient experience. And happy customers (i.e., patients) tend to let others know about the great compassionate care they received from a particular organization. Likewise, unhappy customers are all too willing to let others know about their bad experience.
Own the process
Lastly, one of the most important parts of the interview is how the interviewer conducted himself. We are the face of the organization we work for. We need to respect the person who applied for a job and visited the organization seeking a job. Yes, most of us are busy and sometimes we have to squeeze an appointment in between a mountain of other things to do. But as interviewers we should remember that the impressions we leave with applicants are very important. Always remember there is person sitting on the other side of the desk and our decision to hire or not hire can definitely change her life.
We all want to find the best employees for our organizations. Sometimes it’s tough to find the right person, and in some situations, we may have to settle for people who might not be the best fit. But taking the time to understand and own the process might help in finding the most suitable candidate that is available.
Reference
- A message from Steve Wynn. http://wynnjobs.com/mobile/index.php.
What’s on Your Mind? An AARConnect Discussion Forum Survey
John S. Rinck, MM, RRT-NPS, CPFT
Adjunct Faculty, Graduate and Professional Studies, Spring Arbor University, Traverse City, MI
The AARConnect Management Section Discussion Forum provides an insightful view into the concerns of today’s respiratory therapy services manager. Daily postings in the Discussion Forum provide a broad and interesting view into issues that matter to managers across the health care spectrum. Anyone following daily postings soon develops an understanding of the breadth, depth, and complexity of the issues that face managers in today’s health care environment.
Of particular interest is the seemingly high number of posts related to equipment. Devoting time and decision-making resources to equipment-based issues potentially restricts involvement and commitment to administrative functions. The question arises when reading daily posts, “How representative are these posts proportionally to what managers actually do?”
Are these posts a true representation of RT management today? Insight into RT management responsibilities can be best understood by formulating an objective and hypothesis, and conducting a survey to potentially clarify and advance the understanding of the RT management function as reflected in the Discussion Forum. I conducted just such a survey earlier this year.
Purpose: The purpose of this mini-project was to survey, record, and categorize the entries made in the AARConnect Management Section Discussion Forum and to provide evaluation and comment about the results as a window into the issues that are of concern to respiratory therapy managers.
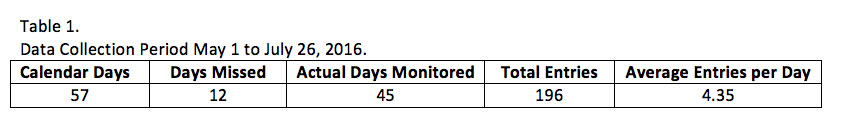
Objective: Between May 31 and July 26, 2016 (57 days), daily Management Section Discussion Forum posts were surveyed, tracked, categorized, and tabulated from the AARConnect site.
Hypothesis: An unusually high amount of daily entries (75% or more) will be equipment focused.
Methods: Daily entries made in the Forum were recorded each day between May 31 and July 26, 2016. All entries during the survey were categorized into one of five functional groups: 1) POCD – Planning, Organizing, Controlling, and Directing 2) Budgeting 3) Staffing, 4) Managing, and 5) Equipment. Percentage and proportion statistics were then determined for functional groups 1-4 (Administrative) and compared to those of functional group 5 (Equipment). Daily entries were surveyed across clinical and administrative lines of responsibility. Demographics, credentials, department titles, positions, and roles were not tracked when recording each entry. Results were tabulated using sample percentages and population proportion statistics at the 95% C.I. to either support or disprove the hypothesis.
Results: Data collection during the survey period is displayed in Table 1.
Daily entries spanned a wide range of subjects: 1) Direct Patient Care, 2) Technology/Equipment Operation, 3) Patient/Staff Safety, 4) Equipment Storage and Inventory, 5) EMR/Documentation, 6) Protocols/Procedures, 7) Staffing, 8) Coding, 9) The Joint Commission, 10) Productivity, 11) Medication Administration. Depending on the information sought, the problem being solved, or the inquiry being made, all entries were divided into one of the five categories listed in Table 2.
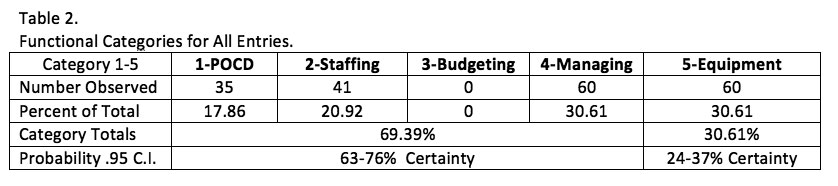
Because only 30.61% of all entries dealt directly with equipment operation, use, set up, or function, the hypothesis statement was rejected. We can predict with 95% certainty that equipment use, setup, or function will occur between 24-37% of the time as a management concern reported in the Management Section Discussion Forum, and issues surrounding administrative functions and duties will occur with 95% certainty between 63-76% of the time.
Discussion: The observations made from this survey include a variety of assumptions that are difficult to avoid. The biggest assumption was to believe that discussions posted in the Forum represent what RT managers are concerned about. Indeed, there are many other details of their work that are not accounted for or evidenced from surveying Forum posts. Further, blurred lines between the five categories used to capture management functions from the Forum were very difficult to categorize with certainty. However, Table 2 emerged as the simplest way to capture and report this interesting data.
The two major divisions separating data collection in Table 2 (Administrative functions and Technical/Equipment functions) emerged from the initial perception of how often they appeared as Forum posts, leading to formation of the hypothesis and eventually to the survey. Not until entries were actually categorized in a frequency table and statistically examined was it possible to confirm or reject the hypothesis.
Does the frequency of each kind of post bear meaning on the management function in respiratory therapy? Are Forum posts reflective of the time devoted to management responsibilities? Results displayed in Table 2 indicate it would be relatively safe to say that managers are spending productive efforts on functions and responsibilities traditionally held as managerial duties. But what is the right amount of time, the proper amount of time, the normal amount of time? Is there such a statistic?
There are numerous angles from which to approach equipment issues. Equipment issues certainly overlap and blend with administrative decision-making: budgeting, management, planning, and controlling, to name but a few. Equipment use clearly is not just a technical issue realized by the therapist at the bedside. However, care was taken during this survey to align Forum postings under the appropriate category based on the underlying issue. For example, equipment procedure development, protocols, education, and resource utilization were categorized as administrative functions (Category 1-4) even though they involved equipment in some way. By doing so, potential bias was eliminated.
Other implications emerge from this survey. First, demographics were not addressed at all. If titles and positions of those seeking input and feedback in the Discussion Forum were considered, would the results have looked entirely different? What portion of the entries surveyed was made by directors, managers, supervisors, staff therapists? It might make a difference in a forum geared to management issues.
Second, thematic presentation and repetition of subjects could be the groundwork for creation of future coursework offered through channels of continuing education.
Third, the absence of budgeting entries in the Forum is interesting, but may indicate that budgeting is fully addressed in the manager’s respective institution with oversight from a director, financial resource personnel, or some other administrative partner.
Fourth, not all entries stated problems; rather many entries offered answers and supplied resources to those seeking answers to their questions.
Conclusion: The AARC may have an existing tracking methodology within the Management Section Discussion Forum on AARConnect and a developed means of categorizing daily entries. The information gathering that takes place from a rich resource such as the AARConnect Management Section Discussion Forum can act as a vital link to professionals at all levels of care and from many diverse backgrounds in the field of respiratory therapy.
Section Connection
Recruit a New Member: Know an AARC member who could benefit from section membership? Direct them to section sign up. It’s the easiest way to add section membership to their overall membership package.
Section Discussion List: Go to the section website and click on “Discussion List” to start networking with your colleagues via the AARC’s social networking site, AARConnect.
Next Bulletin Deadline: March 1.